ABSTRACT
Geriatric patient cases are ideal for use by basic science educators who seek to link key principles and concepts with clinical medicine. However, access to geriatric educators and geriatric patients able to highlight the evolution of a particular disease/condition, limits the basic science educator??bf?s ability to easily incorporate clinical cases into their teaching. To address this resource limitation, we developed five core geriatric clinical cases, each portraying a patient who ages over time, for repeated use in multiple courses/clerkships across the four-year medical student curriculum. In this article, we describe the process involved in designing the cases with illustrative examples of their use in selected basic science courses. Guided by John Kotter??bf?s change process, the project team sponsored a series of invitational workshops composed of basic science and clinical educators whose expertise was related to the patient under review. At each workshop, an abstracted patient record was presented (e.g., longitudinal history, physical exam, laboratory data, and diagnostic images), and participants modified the case to better highlight teaching points associated with their respective courses/clerkships. Each updated case was then circulated to all workshop attendees, and other educators across the curriculum, for incorporation into their instruction. The flexibility of each case enables faculty to use the case(s) in varied settings (e.g., lectures, problem based learning groups, labs) matched to the objectives, resulting in students having a longitudinal experience with five geriatric patients and their diseases. The cases continue to be incorporated into the curriculum with students reinforcing the value of their inclusion as they follow the patient??bf?s diabetes and its progression through biochemistry, physiology, surgery and medicine. In summary, Kotter??bf?s change steps effectively guided the project team and can serve as a model for educators seeking to enhance reciprocal integration of basic and clinical sciences.
INTRODUCTION
Basic science educators have sought to link the principles and concepts of their disciplines with clinical medicine by implementing multiple basic science curriculum structures (e.g., organ-based, discipline-based, key features/problems) and formats (e.g., problem-based learning, clinical correlations, simulations, lectures, laboratories). Yet, only 12% of the 2003 graduating seniors surveyed via the Association of American Medical Colleges (AAMC) Senior Graduation Questionnaire1 strongly agreed that basic science content had sufficient illustrations of clinical relevance and provided relevant preparation for their clerkships.
Simultaneously, clinical educators struggle to facilitate the incorporation of specific topics or populations into the curriculum. For example, because geriatric patients are a critical population in medicine, Dr. Robert N. Butler, the first Director of the National Institutes on Aging, was an early advocate for the exposing medical students to geriatric medicine topics and clinical concepts throughout the medical school curriculum.1 With funding awarded through AAMC/John T. Hartford Foundation, over 40 U.S. medical schools have introduced geriatrics educational initiatives spanning all four years of the curriculum.
The opportunity to integrate clinical geriatrics and basic science is readily apparent as 85% of geriatric patients have at least one chronic illness, most commonly arthritis, hypertension, heart disease, or hearing and vision loss.1 Each of these conditions provides a teaching opportunity to link the foundational principles of basic science with their application in clinical medicine. For example, arthritis provides the opportunity to explore critical concepts associated with anatomy (cartilage), biochemistry (biochemical aspects of connective tissue), and pharmacology (pain management) while diabetes highlights biochemistry and physiology (glucose metabolism, influence of body composition), and microbiology (mechanisms of infection risk). Enhancing students’ ability to articulate the key role that basic science concepts plays in understanding disease mechanisms and the associated assessment and management of patients is the shared challenge facing basic and clinical faculty with limited curriculum and faculty time.
Clinical Continuity within Case-based Instruction
Recognizing that medical students view the incorporation of clinical cases as a common parameter of effective instruction, we sought to collaboratively develop a common set of core geriatric clinical cases that could be used repeatedly in multiple courses/clerkships across the four-year medical student curriculum. By creating a set of core cases, to be utilized by faculty teaching in basic and clinical sciences to illustrate their discipline/specialty specific concepts, an appreciation for geriatric patients as well as their multiple and complex medical problems could be woven throughout the curriculum by non-geriatricians.
The challenge to medical educators in using geriatrics examples is that the curriculum must also address students’ attitudes towards elderly people. Common stereotypes of the old are that they are frail, dependent, reside in nursing homes, and are refractory to medical treatment. In reality, the vast majority of older adults are community dwellers with minimal functional limitations that maintain productive and active lifestyles and seek to remain healthy, actively collaborating in their care.4,5 In order to address this attitudinal dimension and the ability to understand the continuous nature of disease progression over time, we added a unique element to our clinical cases: each patient “ages” across the curriculum to highlight the progression of health and illness in the elderly population. With funding from the John A. Hartford Foundation, geriatric faculty selected five geriatric patients who had common disease presentations to serve as the foundation for our curriculum intervention. Each patient’s findings, over at least a 15-year period of care, were abstracted to create a paper case highlighting common clinical conditions (Figure 1).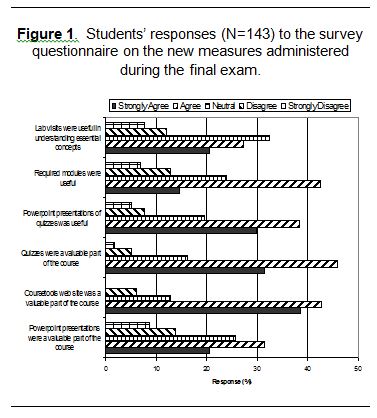
Two challenges faced the geriatric physician educators and the targeted basic scientists and clinical faculty who were intended to adopt and integrate the cases into their existing teaching formats: 1) To what degree did the cases need to be adapted to better match the principles/concepts emphasized for use within the basic science courses and clinical clerkships? 2) What would enhance the likelihood that basic science and non-geriatrics clinical faculty would incorporate the cases within their teaching?
The remainder of this article will describe how collaboration between case authors and a broad base of basic science and clinical faculty was initiated through a series of case consultation workshops. Key features of these workshops will be identified, followed by presentation of preliminary adoption/integration rates by case in the basic science and clinical curriculum.
A Systematic Approach to Curricular Integration Using Case Consultation Workshops
To answer these questions of content and utilization, a 1.5-hour “Case Workshop” was held with an invitation only audience specific to each case. As we were seeking to introduce a change in the way educators select and use cases as part of their instruction, we followed aspects of the eight-step change process outlined by John Kotter: 1) establish a sense of urgency; 2) create the guiding coalition; 3) develop a vision and strategy; 4) communicate the change vision; 5) empower broad-based action; 6) generate short-term wins; 7) consolidate gains and produce more change; and 8) anchor new approaches in the culture.6 Each of these steps will be briefly described to provide a framework that may assist other medical educators in seeking to synergize basic and clinical science education.
Step 1: Establish a Sense of Urgency
As part of the application for the AAMC/Hartford Award, the project staff conducted a needs assessment that revealed limited systematic exposure to geriatrics in spite of its population-based significance for medical education. Upon receipt of the AAMC/Hartford Award, geriatric education became more visible and public at the Medical College of Wisconsin (MCW) as it represented an influx of funds targeted to a broad-based curriculum initiative. The award was announced in college-wide newsletters, websites and at key meetings of medical educators. The two-year timeline provided a critical level of urgency on the part of the project staff, which included some of MCW’s key educational leaders (e.g., Associate Deans involved in undergraduate medical education, Chair of the Curriculum and Evaluation Committee, Division Chief for Geriatrics). In addition, the course/clerkship directors recognized the need to incorporate geriatrics into the curriculum, based on the results of the needs assessment.
Steps 2-3: Create the Guiding Coalition and Develop a Vision and Strategy
As described above, the project team consisted of positional (Associate Deans, Division Directors, Chair of the Curriculum and Evaluation Committee) and influence leaders (members of MCW’s Society of Teaching Scholars). Collectively, these individuals were present at all standing committee meetings related to undergraduate medical education. This “coalition” played a vital role in collaborating with the geriatric educators to develop a vision and strategy for designing and implementing the case-based approach to geriatric education. Key features of this strategy included targeting faculty already teaching about the topics associated with a particular aspect of a case, inviting those faculty to participate in the development of each case to insure that it met their needs as instructors, and providing those instructors with the flexibility to adopt/adapt the case(s) to meet their needs. Furthermore, a steering committee of key basic science and clinical faculty opinion leaders was convened to oversee the effort of the project team. This group guided the project team and made suggestions to ensure meeting of project goals.
Steps 4-5: Communicate the Change Vision and Empower Broad-Based Action
The project team and key faculty in each basic science and clinical clerkship associated with an aspect of each case met together for a brainstorming session. For example, the case of Mr. Karl Andrews (Figure 1, Case 1) highlighted diabetes, lipids/cholesterol, coronary artery disease, medications, genetics, hypertension, stroke, informed consent, and rehabilitation. Faculty responsible for teaching glucose metabolism (biochemistry, physiology), lipid formation/cholesterol (biochemistry), imaging (radiology) and rehabilitation (physical medicine and rehabilitation) were among the faculty targeted for invitation. A group e-mail was forwarded to all invitees explaining the project and the need for their input to ensure the case was congruent with the core principles highlighted in their instruction. A personal contact from the project team member who best knew the faculty member followed the initial e-mail invitation.
The result of this targeted and personally invited attendance approach was a broad-based representation of basic science and clinical specialties at each of the five case workshops. Each workshop began with a brief overview of the project, emphasizing the need to adapt the core case so that it could be incorporated into teaching the concepts faculty were already presenting in their instructional units. For example, in the case of Mr. Karl Andrews who begins as a functional 65 year old with multiple risk factors for atherosclerosis including diabetes, the biochemist contributed insights into the pathophysiology of glucose metabolism while the physiologist focused on endothelial cell effects of prolonged hyperglycemia that explains subsequent clinical phenomena in terms of signs and symptoms. To heighten these points, the case was slightly revised to enable the physiologist to incorporate it into his existing core lectures. However, since the educational needs of the instructors did not always coincide, dynamic dialogue about clinical phenomenon and the science ensued. As the geriatrics division chief commented, “This was really fun! For the first time in 20 years of medicine, I had participated in dialogue about medical education. It’s not that I don’t see these people at committee meetings. (But there) we talk about rank and tenure, faculty fringe benefits, not the science of medicine. And this was all that we did. It was very exciting”. The success and “fun” of participating in the first case workshop provided a “short term win” that allowed the project team to continue to use the case workshop format to, in Kotter’s terms, communicate the change vision and empower broad-based action.6
At the conclusion of the discussion, each individual’s key issues were incorporated and faculty members were advised that a final draft of the case would be circulated for review. Following the meeting, the clinician members of the project team finalized the case to insure that changes in findings at age 65 were consistent with disease progression/findings as the patient aged to 70, 75, 80, etc. The updated case was then circulated to the workshop attendees individually and through the course and clerkship director’s and the Curriculum and Evaluation list serves.
Steps 6-7: Generate Short-Term Wins, Consolidate Gains and Produce More Change
Following the short-term wins stemming from each case workshop, faculty enthusiasm for incorporating the cases was high. Almost immediately, Cases 1 and 2 were incorporated into first-year basic science courses and into the required M3 medicine course. As students began to recognize Mr. Andrews (Case 1) and Mrs. DuBois, (Case 2) in subsequent courses/clerkships, the faculty recognized that the continuity approach to case presentation was effective in providing students with a relationship with these patients. The flexibility allowed by encouraging instructors to just “mention” the case by the patient name as an example of concepts addressed in class ensured that instructors maintained the autonomy and control over their content that other curriculum change approaches often preclude.
Short-term wins were also celebrated by dissemination of how each course was using the cases at regular meetings of the course and clerkship directors. Recognition was provided in an ongoing manner as each course/clerkship implemented the use of the cases. For example, when Mr. Andrews” case was implemented, its use in biochemistry during discussions of glucose metabolism and later cholesterol metabolism was announced. Physiology was recognized when it used Mr. Andrews to highlight the physiology of diabetes. Surgery was able to use the case in discussing the ankle/brachial indices used to assess vascular disease and Internal Medicine used Mr. Andrews to highlight various clinical aspects during a required clerkship. The implementation of a fourth-year elective centered exclusively on four of the cases was another cause for celebration and recognition. These announcements and recognition continued as each new case was introduced and often resulted in discussion about how the case could be used in other areas.
Step 8: Anchor New Approaches in the Culture
As the cases became finalized, the instructors could choose to incorporate any aspects of the case into their teaching. While dependent upon the decisions of each faculty member, the degree to which core curriculum topics are subsequently revised is limited from year to year. When changes are made, the flexibility of the continuity case structure and the availability of cases highlighting most common issues in the aging provide a strong anchor to sustaining case utilization within the curriculum. An example of how multiple cases have been used in a single course, cell and tissue biology, is presented in Figure 2. 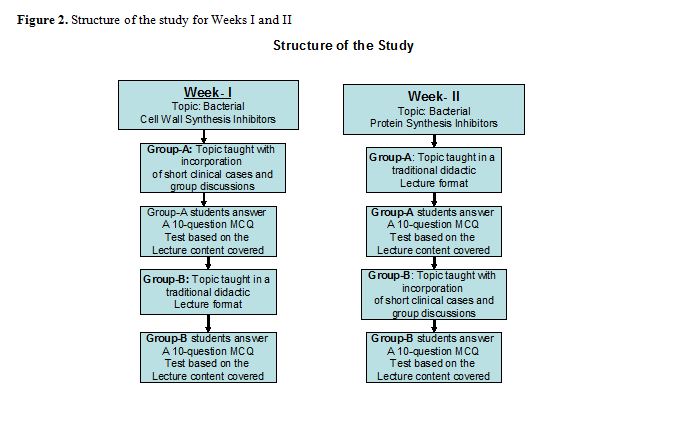
First-year students are now introduced to all the cases during orientation. In this orientation session focused on the medical school curriculum, each patient is identified and associated with the primary disease processes with which they will be associated. The concept of the patient aging as the student encounters them throughout the curriculum is also explained.
To solidify the use of the cases, the project team also took advantage of additional opportunities to embed the cases within the medical student curriculum. One such opportunity was MCW’s M1-2 Integrated Rounds, a program sponsored by the M1-2 Course Directors, the MCW Society of Teaching Scholars and the local student chapter of the American Geriatrics Society. This collaborative one-hour session featured a clinical geriatrics faculty member and two basic science faculty members (pharmacology and microbiology) and centered on Mr. Malone (Case 3 depression/dementia). The clinician presented the case and led an interactive session with the medical students generating a differential diagnosis and emphasizing clinical features of the case. The microbiologist then presented background data on one of the possible transmissible causes of dementia listed in the differential of the case and the pharmacologist focused on antidepressant classes and the most efficacious therapy for depression in the elderly. Over 150 students attended the session with very positive evaluations specific to integrating basic and clinical science within the curriculum.
A second opportunity to embed and solidify the cases was through the creation of a required selective in geriatrics. Students are given the written cases in their entirety, rather than the selected elements highlighting the targeted basic science and/or clinical-specific foci approach experienced during the first three years of the curriculum. One case is highlighted during each week of the month-long selective. Each week students individually choose a “learning issue” that highlights some aspect of basic pathophysiology in the case. Thus, this selective provides an opportunity to revisit basic science concepts during the fourth year. Each student then presents the “learning issue” to his/her peers under faculty guidance, which includes basic and clinical faculty. In addition, a clinical interaction with a standardized patient based on the case allows the students to synthesize their knowledge and apply it in a clinical interview.
Preliminary Evaluation Results and Next Steps
All five-paper cases have been finalized and successfully integrated into the curriculum. Over two-thirds of the basic science courses have incorporated at least one case as of the 2001-02 year with case five introduced at the very end of that academic year (see Figure 3). Results from the 2003 AAMC Senior Graduation survey reveal a strong positive shift in the perceived relevance of our basic science content moving from a rating of 3.0 in 2001 (1 = Strongly agree; 2 = Agree; 3 = No Opinion) to 2.7 in 2003 (national mean 2.6). The perceived validity of basic science content as relevant preparation for clerkships also shows a promising trend moving from 2.8 in 2001 to 2.5 in 2003 (national mean 2.5). While a number of other initiatives have been implemented that can contribute to these ratings, in their narrative comments students commonly cite geriatrics as an example of clinical relevance. 
To maintain our momentum around the longitudinal geriatric case approach and to respond to instructors’ requests to make the patients “live”, we are in the process of re-creating each case as a CD-ROM-based teaching resource file for instructor use with the support of the Donald W. Reynolds Foundation. Each CD will contain 1-2 minute video clips portraying the patient interacting with a physician, other health care providers, or family member(s) at each of the major age periods to highlight key clinical findings. The video clips are then incorporated onto a CD-ROM along with radiographic images (e.g., bone density scans), still images (e.g., diabetic ulcerated toe, recurrence of breast cancer nodules), and assessment findings (e.g., mental status examination, functional status examination). Each image is then linked to the associated topic and indexed by common basic and clinical science courses/clerkships to allow easy access by faculty to a virtual patient record.
SUMMARY AND CONCLUSIONS
A continuity case-based approach can be successfully used to highlight the sciences basic to medicine across all four years of the curriculum. Guided by Kotter’s eight-step change model, a systematic case development approach was implemented that has successfully incorporated geriatrics into our curriculum and can serve as the model for enhancing the clinical relevance of our basic science courses and revisiting basic sciences in the clinical curriculum.
REFERENCES
- Medical school graduation questionnaire 2003. Washington, D.C.: Association of American Medical Colleges, 2003. Question no. 7
- Butler, R.N. Selected as best paper in Journal of the American Geriatrics Society in the 1970s mission of the National Institute on Aging. Journal of the American Geriatrics Society. 2003; Aug; 51(8): 1169-73.
- Trends in aging-United States and worldwide. Morbidity and Mortality Weekly Report. 2003; Feb 14; 52(6): 101-104, 106.
- Alliance for Health Report. Chronic care. In: Covering health issues: 2003-a sourcebook for journalists. Available from: http://www.allhealth.org/sourcebook2002/ch10_1.html. Accessed August 13, 2003.
- Administration on Aging. A profile of older Americans: 2002. Washington, D.C.: U.S. Department of Health and Human Services, Administration on Aging, 2002.
- Kotter, J.P. Leading change. Boston: Harvard Business School Press; 1996.