ABSTRACT
This study tested the hypothesis that practice pelvic examinations on teaching patients within the second year medical school curriculum improve student perceptions of competency and preparedness for clinical rotations. After IRB approval, 260 second year medical students were asked to complete two voluntary, anonymous electronic surveys: one prior to their practice exam and one afterwards. Eighty-eight students (34%) completed the pre-exam survey; 76 students (90%) indicated they never had performed a pelvic exam. Seventy-one students (27%) completed the post-exam survey. Before the activity, 39 (45%) students did not know how to use a speculum; 57 (67%) could not bi-manually locate the cervix; 69 (81%) could not bi-manually locate the uterus; 72 (85%) could not bi-manually locate the ovaries; 74 (87%) could not assess pubococcygeus muscle tone; and 31 (36%) students were not familiar with the appearance of a cervix. Following the experience, 71 (100%) students knew how to use a speculum; 70 (99%) could bimanually locate the cervix; 66 (93%) could bimanually locate the uterus; 57 (80%) could bi-manually locate the ovaries; 44 (62%) could assess pubococcygeus muscle tone; and 70 (99%) students knew what a cervix looked like. Students indicated that the practice pelvic exam improved their perception of preparedness (n=70, 99%) and confidence (n=64, 90%) for performing the pelvic exam and 64 (90%) students reported that the experience helped reduce their anxiety about performing pelvic exams. The practice pelvic exam activity considerably improved student self-perceived competency and preparedness for clinical rotations, which may help their future performance.
INTRODUCTION
Physical examination and communication skills are important components of medical education that are typically taught throughout all four years of medical school. However, the female pelvic exam is a component of the physical exam that is often not adequately addressed in the curriculum; this exam is especially challenging to teach and to learn because of its sensitive nature.1 Medical students often have limited or no opportunity to practice the pelvic exam during the first two years of medical school. Furthermore, opportunities to practice this exam during clinical rotations may be limited due to patient preference, student or preceptor gender, and practice type.2,3 The exam can be uncomfortable for both the patient and the medical student. There are also ethical concerns as to whether students should perform their first pelvic exam on a clinical patient.4 Several studies suggest that in some clinical circumstances, students do not receive the necessary degree of clinical exposure for them to be able to enhance their knowledge and gain competency in specific skills.5 There is no consensus about the number of pelvic exams required to be competent; however, it is often assumed that increased experience correlates with increased competency and confidence.1
It is important for students to learn clinical skills in an environment in which they are able to receive instructions, ask questions, integrate their medical knowledge with clinical skills, and practice communicating with patients. Standardized Patients (SP) and Teaching Patients (TP) have become an increasingly integral component of medical education; they play a role in both the teaching and assessment of student clinical skills.6 SP are paid to simulate a clinical scenario, in order for students to practice taking medical histories, performing physical exams, and treating the patient. The TP role is to guide the student through specific clinical and communication skills, rather than simply role play. Some medical programs use SP and/or TP, who actively participate as teachers, to assist students in developing their clinical and communication skills for performing pelvic examinations.7 There is limited research on the effect and outcome of using SP and/or TP to facilitate this type of clinical learning experience. In addition, the timing of the SP and/or TP experience in relation to student medical school year varies; some programs take place immediately before obstetrics and gynecology clinical clerkship, while others begin earlier in the students’ medical education.4,7
Currently, practice pelvic examinations involve use of the speculum, components of the bimanual examination, and appropriate physician-patient communication. Unlike physical examination components, the sensitive nature of this examination can make medical students unnecessarily nervous and therefore it can be difficult for them to communicate and work effectively. The use of SP throughout the first 2 years of medical school is quite common, considering the assumption that increased experience correlates with increased competency and confidence.1 However, the underutilization of practice pelvic examinations within the first 2 years of medical school leaves students vulnerable. Therefore, the purpose of this study was to examine the effectiveness of practice pelvic examinations by evaluating student- reported clinical and communication competency before and after the experience. We hypothesized that practice pelvic examinations on teaching patients, within the second year medical school curriculum, would improve students’ perceptions of competency and preparedness for clinical rotations.
MATERIALS AND METHODS
Sample
The 260 second year students at Kansas City University of Medicine and Biosciences (KCUMB) were asked to complete voluntary pre- and post-exam questionnaires regarding their experience during a practice pelvic exam activity. Students were required to practice the pelvic exam in a controlled teaching environment during the Reproductive section of their second year medical education. This section lasted six weeks, and it was the last academic section before students began their clinical clerkships. During the first week of the reproductive section, students were instructed how to perform the pelvic exam and what to expect during the practice exam experience; students were required to participate in the simulation once.
Survey questionnaire
The electronic questionnaires were released during the second week of the Reproductive section, before the simulated experiences began. The questionnaires were validated by a small sample of individuals before being released. Students were informed verbally and electronically via email about the voluntary survey. The survey was posted to the Blackboard online student forum and students were responsible for completing the surveys before and after their simulated experience, within the time frame of the six week section. The survey was completely voluntary and student responses were anonymous.
To protect the identity of our students, minimal questions were asked concerning demographic information. The pre-examination (pre-exam) questionnaire included eighteen questions regarding gender, perceptions of the pelvic exam experience, previous pelvic and breast exam experience, what skills the students already had for the pelvic examination, and self-assigned code number. The post-exam questionnaire consisted of forty-one questions; ten of the pre-exam questions were repeated in order to determine whether the pelvic exam simulation had an impact on student self-perceived ability to perform the pelvic exam during a clinical rotation. Additional questions concerning the organization of the pelvic exam experience, and perceptions regarding how the simulated pelvic exam experience prepares them for future clinical rotations were added to the post-exam survey. The participant’s response option was based on the following 5 point Likert scale: strongly agree, agree, neither, disagree and strongly disagree.
Statistical Analyses
Due to lack of student recall of their self-assigned code number, pre-exam to post-exam comparison was not plausible. Therefore, pooled descriptive statistics are reported for each survey.
RESULTS
There were 260 students in the second year medical class. Of the 260 students, 88 (33%) completed the pre-exam survey (36 male, 51 female); of those, seventy-six students (90%) had not performed a pelvic exam previously. Seventy-one (27%) second year medical students completed the post-exam survey (32 male, 34 female).
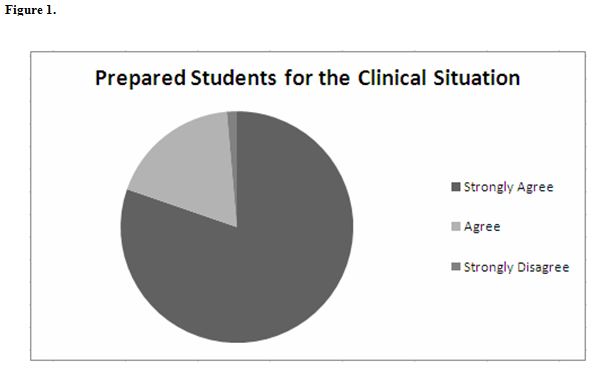
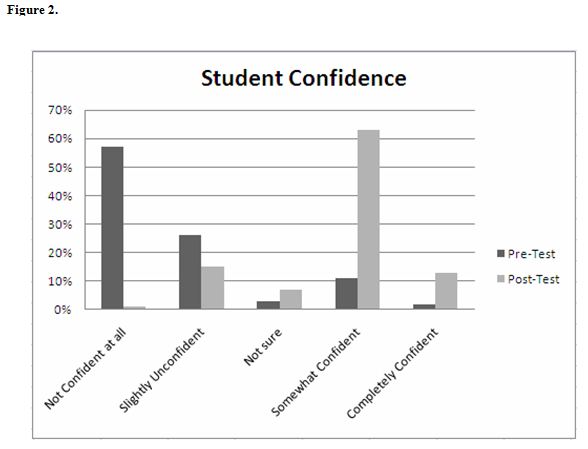
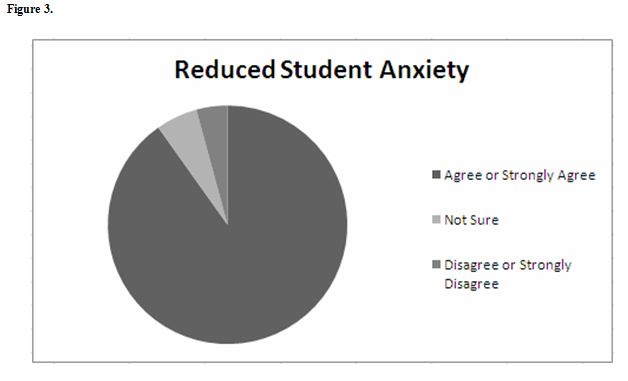
Summary data indicates that the simulated pelvic exam significantly improved student preparedness (n=70, 98%) (Figure 1) and confidence (n=64, 90%) to perform the pelvic exam in the clinical situation (Figure 2). In addition, 64 (90%) students reported that the simulation helped to reduce their anxiety about performing the pelvic exam (Figure 3).
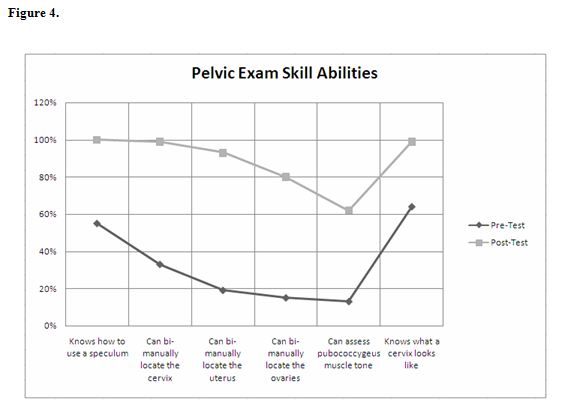
Before the practice examination experience, 39 (45%) students did not know how to use a speculum; 57 (67%) could not bi-manually locate the cervix; 69 (81%) could not bi-manually locate the uterus; 72 (85%) could not bi-manually locate the ovaries; 74 (87%) could not assess pubococcygeus muscle tone; and 31 (36%) students did not know what a real-life cervix looked like.
Following the pelvic exam simulated experience, 71 (100%) students knew how to use a speculum; 70 (99%) could bi-manually locate the cervix; 66 (93%) could bi-manually locate the uterus; 57 (80%) could bi-manually locate the ovaries; 44 (62%) could assess pubococcygeus muscle tone; and 70 (99%) students knew what a real-life cervix looked like (Figure 4).
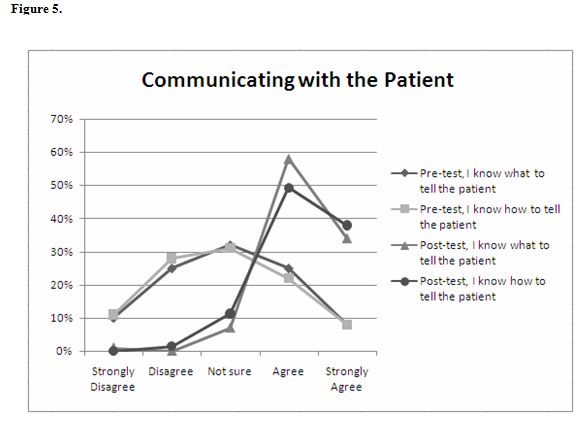
The student ability to communicate with the patient about the pelvic exam procedure was also assessed in the pre- and post-exam surveys. Before the practice experience, 30 (34%) and 27 (31%) students indicated that they were not sure how to explain and what to tell the patient concerning the exam procedures, respectively. However, after the practice pelvic exam experience, 62 (87%) and 65 (92%) students agreed or strongly agreed that they knew how to explain and what to tell the patient concerning the exam procedures, respectively (Figure 5).
Sixty-nine (97%) students indicated that the pelvic exam activity was well organized. Seventy (98%) believed the experience was a useful way of teaching the pelvic exam. Fifty-nine (70%) students believed this method of teaching promoted teamwork. Fifty-seven (81%) students reported receiving appropriate feedback about their performance of the pelvic exam.
DISCUSSION
Overall, the students indicated very positive feelings about the effectiveness of the practice pelvic exam experience. The physicians and teaching patients provided the students with an appropriate level of instruction necessary for the students to gain the skills required to perform this type of exam. As a result, the students felt more prepared, more confident, and less anxious about performing a pelvic exam in the clinical setting.
The survey results support our hypothesis that the practice pelvic exam activity utilizing Teaching Patients at KCUMB improves second year medical student perceived competency and confidence in performing a female pelvic exam. The TP helped to facilitate a safe environment in which students were able to ask questions, practice skills, and gain exposure to potentially uncomfortable clinical situations. The TP and physician also provided the students with formative feedback regarding appropriate clinical and communication skills.
As a result, the students were able to learn how to perform specific exam skills, such as locating the cervix and ovaries, using a speculum, and assessing pubococcygeus muscle tone. After this experience, the students felt more prepared and confident to communicate appropriately with the patient during the exam.
Several other studies have demonstrated the importance of providing students with hands-on clinical experiences in order to improve their level of confidence and competence.
These studies have determined that this type of practice experience is a significant independent predictor of student confidence.5 Our results support this conclusion. However, the relationship between self-perceived clinical competence and actual clinical competence or performance cannot be determined from this study. Although students reported that they felt prepared for and confident in performing a pelvic exam during clinical rotations, there was no direct assessment of their preparedness in rotations. Because the students did not receive a grade following the practice experience, no correlation can be made between their performance during the practice exam and their performance during clerkships.
Previous studies suggest that there is no correlation between clinical experience or confidence and measured performance assessment, including both clinical and written examination grades.5 However, the explanation for this result is still unclear. Research by Morgan and Cleave-Hogg suggests that the lack of correlation could be due to several factors, including the quality of the learning experience, the quality of the feedback received during skill acquisition, or how important learning this skill was perceived by the student.5 Our students, however, reported that activity was well organized, was a useful way of teaching the pelvic exam, that this method of teaching promoted teamwork, and that they received appropriate feedback about their performance of the pelvic exam. In addition, students found the teaching patient to be a good teacher and believed the experience provided a supportive learning environment.
Based on our results, we believe that further investigation between clinical experience or confidence and measured performance assessment is warranted. Because the students only received hands-on experience with performing pelvic exams, a correlation using their obstetrics and gynecology clerkship grade, may not provide an accurate point of comparison; students would need to be specifically graded on their pelvic exam performance, in order to have a point of equal comparison. Currently, these data suggest practicing a sensitive type of examination utilizing live teaching patients is beneficial to the students’ feeling prepared for clinical rotations. These data may apply to other sensitive nature exam, such as the male prostate examination.
Limitations
This study had several weaknesses. Due to lack of recall of their code number, we were unable to perform statistical comparisons between surveys. Because the surveys were posted individually, participation on one was not required for the other and without code numbers to match the survey respondents, the pre- and post-survey respondent groups may have consisted of different individuals from the class. Thirdly, since we did not assess student interest in this subject, this factor may have influenced the students’ motivation to participate in the survey and interest in the pelvic examination experience overall. The lack of response may be due to lack of interest or lack of time. This questionnaire took place during the last section of the second year curriculum when most students have the least amount of time due to regular course work, preparing for rotations, and studying for their upcoming board examinations. Lastly, the students who participated in the pre-survey and post-survey, respectively, may not accurately reflect the experiences of all 260 second year medical students who participated in the practice experience or medical students in general.
CONCLUSIONS
Despite these limitations, our study strongly suggests that teaching the pelvic exam during the second year of medical school curriculum helps students to adequately learn the necessary skills needed to perform pelvic exams in the clinical setting. The opportunity to learn the components of this exam in a controlled, supportive learning environment helps students to feel more comfortable and confident in their ability to perform the pelvic exam. Ultimately, the researchers believe that this opportunity, during the second year of medical school, serves as a foundation upon which students can begin to acquire the skills necessary for competency in performing the female pelvic exam.
Future studies
Since the survey was conducted prior to clinical clerkships, it was not possible to determine the degree to which the practice experience actually prepared students for the clinical setting. In order to assess the degree to which the experience actually prepared students for clinical rotations, a follow-up questionnaire is being conducted of all third and fourth year students who have performed at least one pelvic exam during clinical rotations.
ACKNOWLEDGEMENTS
This research information has been presented in poster form at the 2008 American Osteopathic Association Annual Conference, and in oral form at the 2009 KCUMB Research Symposium. The abstract of this manuscript has been published in the Journal of the American Osteopathic Association (JAOA).
This research involved the use of human participants. Exempt status IRB approval from Kansas City University of Medicine and Biosciences was granted for this project before surveys were distributed to participants.
REFERENCES
- Powell, H,S,, Bridge, J., Eskesen, S., Estrada, F., Laya, M. Medical students’ self-reported experiences performing pelvic, breast, and male genital examinations and the influence of student gender and physician supervision. Acad Med. 2006; 81(3):286-289.
- Levy, B.T., Merchant, M.L. Differences in clinical experiences based on gender of third-year medical students in a required family medicine preceptorship. Acad Med. 2002; 77(12 Pt 1):1241-1246.
- Wolfberg, A.J. The patient as ally – learning the pelvic examination. N Engl J Med. 2007; 356 (9):889-890.
- Wanggren, K., Pettersson, G., Csemiczky, G., Gemzell-Danielsson, K. Teaching medical students gynaecological examination using professional patients-evaluation of students’ skills and feelings. Med Teach. 2005; 27 (2):130-135.
- Morgan, P.J., Cleave-Hogg, D. Comparison between medical students’ experience, confidence and competence. Med Educ. 2002; 36(6):534-539.
- Stacy, R., Spencer, J. Patients as teachers: a qualitative study of patients’ views on their role in a community-based undergraduate project. Med Educ. 1999; 33(9):688-694.
- Carr, S.E., Carmody, D. Outcomes of teaching medical students core skills for women’s health: the pelvic examination educational program. Am J Obstet Gynecol. 2004; 190(5):1382-1387.