THE PROBLEM
I will assume that biochemistry is a fundamental building block in the foundations of medical education and that not only is it required to understand many of the disciplines which underpin medicine but that a basic knowledge is required in clinical practice. However, it is right that we should ask ourselves a challenging question even if it is clearly a minefield where each word has to be stepped on carefully. How the question is answered will be influenced by assumptions that biochemical and medical educators have about the nature and function of biochemical knowledge. But the question is not just about “how much??, it is also about the quality, the context, and the utility of biochemical knowledge and the process by which it is acquired.
Medical students have acquired their biochemical knowledge in a variety of ways over the years. The “traditional” method was to teach it as a separate subject as part of a preclinical basic medical sciences course which included, for example, anatomy, physiology and pharmacology. “Integrated” courses attempted to combine biochemical studies with other preclinical disciplines so that the cardiovascular, respiratory and nervous “systems” could be taught. The relatively recent development of the “Problem-Based Learning” approach begins with clinical problems and scenarios and facilitates students in finding out appropriate and clinically relevant knowledge for themselves.
EVIDENCE
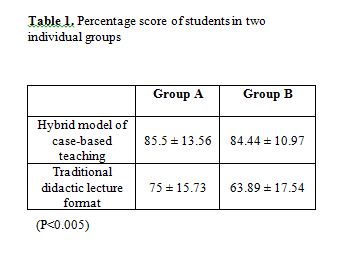
Unfortunately there have been no educational studies which have attempted to compare and evaluate the acquisition of biochemical knowledge via the three models described above. However a study by Clack (1994) on five cohorts of King’s College medical graduates in the UK evaluated how well they perceived the various components of their undergraduate course had equipped them for medical practice. In particular they were asked to evaluate the level of factual content provided by a range of pre?clinical courses. The results are shown in Table 1. The most striking feature of this study is the large number (79.5%) of doctors who perceived that there was “too much” biochemistry in their “traditional” basic science course.
Clearly there is a perception that there is simply too much biochemistry taught in conventional medical courses. Furthermore doctors in the King’s study commented that not only were they taught a “vast quantity” of detailed biochemistry with a “lack of clinical relevance” but that this led to excessive rote learning for examinations.
I recently attempted to replicate this study by a “straw poll” to two medical user groups on the Internet, namely PBLIST and DR-ED. In addition to a number of background questions physicians were asked to rate if they were taught “too much?, “enough?, or “not enough” of the following basic medical sciences. Twenty-three medically qualified people responded. They had been qualified on average for 20 years and 87% had attended a “traditional” medical school. The results are shown in Table 2. Once again, on this much more limited survey, it is apparent that respondents (57%) feel that too much biochemistry is taught in medical courses.
EXPLANATION
As mentioned earlier, the quality, the context and the relevance of this knowledge are important factors influencing students and doctors perceptions.
A possible explanation for these results therefore is that detailed factual biochemical knowledge taught out of clinical context will be perceived as irrelevant and “too much”. So although we can identify a large population of physicians who claim they were taught too much biochemistry it is probable that in “traditional” medical schools they were also taught it out of context.
Current educational thinking suggests that students will learn more effectively if the knowledge and skills acquired are embedded and contextualised in relevant real-life, problem-based situations. Learners build up meanings brick by brick, attaching one concept to another, making connections between concepts, integrating larger conceptual structures and seeing patterns and relationships between concepts. If new knowledge can be successfully integrated, connected and associated with existing knowledge by being relevant, well timed and contextualised then the student’s mental representation expands and deepens leading to “deep level” learning. Such knowledge is more likely to be utilized in applications to new situations and is more useful in solving real problems.
However, if new information cannot be integrated, because it is not relevant, or because it is given at the wrong time the only way it can be retained is by memorization. This type of learning is known as superficial or “surface level” learning and is of limited value in problem-solving. Its acquisition can be tested by recall type examinations, but because it is not completely integrated with existing knowledge it is more likely to be forgotten.
ANSWER
The answer to this problem clearly is to reduce and define the “core” of biochemical knowledge and skills and teach it in an active and student-centered way with emphasis on clinical relevance.
DEFINING A CORE
There is certainly a core of biochemical knowledge that underpins the basic medical sciences and which needs to be learned for an adequate understanding of these disciplines. At the same time it is necessary to look at what biochemistry the practicing clinician needs to know and work backwards to construct an appropriate clinically relevant curriculum. This implies that clinical biochemists and metabolic physicians should be more involved in defining the medical biochemical curriculum. Basic biochemistry learning needs clinical relevance but clinical studies should also be associated with relevant biochemistry. Hence, there needs to be a “bottom-up” and a “top-down” approach to defining the “core”.
NEW WAYS OF TEACHING
Biochemistry needs to be taught from a clinically relevant and contextualised perspective which encourages deep learning. There are many different ways in which this can be achieved. Problem-Based Learning is one approach, but even if not all medical schools adopt this model it is clear that within conventional and integrated medical schools there are many opportunities to reduce didactic teacher-centered learning and replace it with more active, student-centered, clinically relevant teaching.
REFERENCE
Clack, G.B., 1994. Medical Graduates Evaluate the Effectiveness of Their Education. Medical Education 28: 418-431
STRAIGHT OUT OF THE FORTUNE COOKIE JAR …
“The road to success is always under construction”
Anonymous