ABSTRACT
There is increasing recognition that experiences to help students integrate the basic sciences and clinical reasoning should be incorporated into the medical school curriculum. Many schools have adopted case study methods for this purpose in the pre-clinical years but the attempt at integration is often incomplete with failure to return to basic science after clerkships. The Medical Literature Curriculum was developed to integrate the curriculum throughout medical school by study of the medical literature as formal coursework. In the pre-clinical years, students read published case reports, while after clerkships, students read reports of clinical and translational research to return attention to the scientific basis of medicine. The program features guided independent study and large-group discussion with expert clinicians and basic scientists with the goal of modeling, from the first day of medical school, high-level clinical reasoning and the use of basic science knowledge in the discussion of clinical problems. The program has progressively grown as a feature of the required curriculum at our school. It has involved participation by faculty from nearly every clinical and basic science department and provides students with a strong message that reading the medical literature is an integral activity of the profession.
INTRODUCTION
Helping students integrate the basic sciences and clinical reasoning is an important goal for medical school curriculum planning. Introduction of case study into the pre-clerkship years is an approach used by many medical schools as a step toward this goal. The impetus for the widespread adoption of problem-based learning (PBL) is that studying clinical cases brings the basic sciences to life by highlighting their relevance in understanding disease and its management. What has been harder to achieve is a method to bring students back to a focus on the sciences after their clinical experiences in the clerkships.
In this paper, we describe a curriculum innovation that we have developed to promote integration based on the belief that a true integration of science and practice must follow from immersion in the authentic conversation of medicine represented in the medical literature. The attempt to put this into practice has led to an approach to case study in the pre-clerkship years that differs significantly from PBL and to an extension of the experience beyond case study for a return to the scientific basis of medicine in the fourth year of medical school.1 The essence of the program is study of selected papers from the medical literature as formal coursework. We discovered early on that published case reports provide an accessible entry into the literature for beginning students and, like case study by other methods, are a means to motivate and energize pre-clerkship students and faculty.2 After establishing a method for studying case reports as required courses, we recognized that the approach also provides a vehicle for studying primary clinical and translational research reports later in training.3 The method we have devised takes advantage of an unending stream of up-to-date material and utilizes large-group class sessions. These features give the program a limited cost and flexibility that allows relatively simple incorporation into most curriculum structures.
The Medical Literature Curriculum
The Medical Literature Curriculum (MLC) is a series of courses consisting of directed study of papers in mainstream medical and scientific journals. The courses run in parallel with the standard medical school curriculum throughout years one, two and four of the four-year program at SUNY Upstate College of Medicine, Syracuse, NY, and successful completion of these courses is a requirement for graduation. All three courses consist of active learning experiences comprised of: 1) independent study of assigned papers, 2) large-group class discussions of the papers with faculty experts in the areas of interest and 3) written assignments directed at specified learning objectives. Initially, during the pre-clinical years, students are directed to read published case reports to balance and promote integration of the basic science curriculum. After the clerkship experiences, students return focus to the scientific basis of medicine by studying reports of biomedical research. Throughout this extended experience, students are expected to develop increasingly sophisticated explanations and to bring ever-deepening formal analytic knowledge to their experiences.
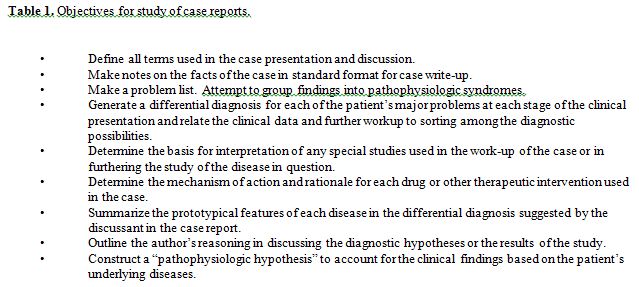
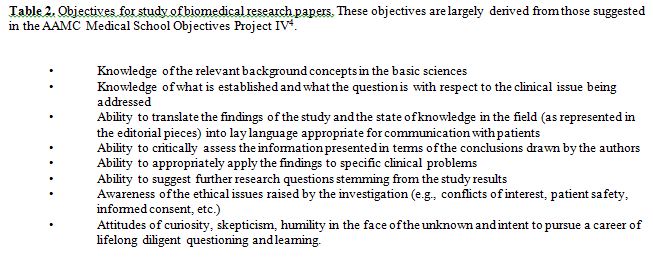
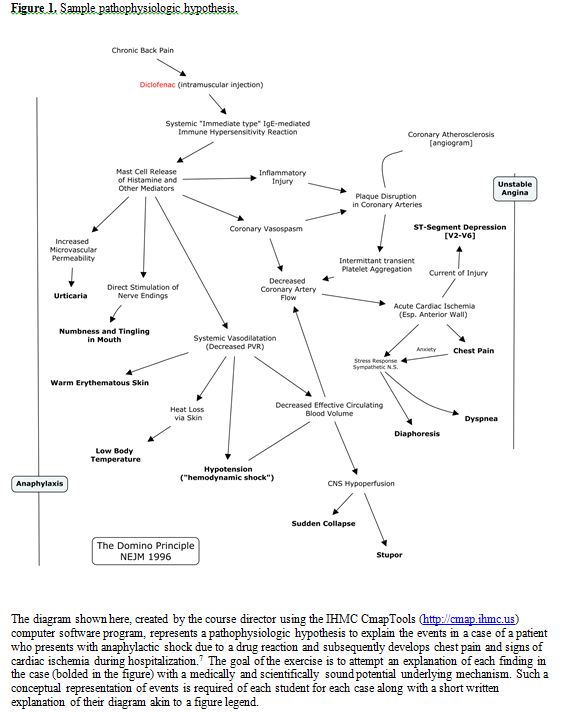
The specifics of the methods of the program follow from the major educational goal, namely to engage students in an authentic, contemporary discussion of medicine and its supporting disciplines at the highest level possible. The assignments, the type of student-faculty interaction and the means of assessment are all designed with the intent of guiding students into that discourse. The papers themselves provide a scaffold and a target for learning. They model exemplary clinical reasoning or research approaches, showing students what a skilled physician or clinician-scientist should be capable of. The specific issues raised in the readings guide students toward filling gaps in their understanding from very basics to the edge of current understanding and into the heart of ongoing discussion of open questions. Further direction is supplied by faculty participation in discussion sessions. Using the large-group setting makes the expertise of the faculty and some uniformity of experience available to all students. The role of the faculty is to provide some additional perspective from their experience in the area of focus in the paper, oftentimes by means of some introductory comments, but ideally, the main role of faculty is to interpret and redirect the questions of students and to assure that the discussion stays on a productive course. Assessment is through “open notes” quizzes prior to class discussion directed at ensuring participation in the process. In this format, students are allowed to make use of any handwritten notes they have made while reading the paper or while doing background research either alone or in collaboration with peers. Specific objectives given to the students to help define their task while reading cases are given in Table 1 and for research reports in Table 2. The design of the quiz questions focuses on whether the students have taken adequate paths in gathering information needed to understand the specific case or research report rather than whether they have mastered some generalized body of knowledge. Question stems include phrases like “in this patient” so that even a knowledgeable physician who has not read the paper would be unable to answer them, and likewise, a student who has read the paper but has not further investigated the issues according to the stated objectives would not succeed (e.g., merely making note of the name of a drug used but not exploring the indication for its use or mechanism of action). Written assignments are submitted after the class discussion. For case studies, the assignment is to generate a conceptual “pathophysiologic hypothesis” that explains the clinical phenomena in terms of underlying disease mechanisms (an example is given in Figure 1). After submission of their hypotheses, a follow-up class session, usually led by the course director, explores a range of reasonable explanations of the phenomena in the case. Afterwards, students evaluate and grade each other’s hypotheses. For research papers, the written assignments are aligned with the objectives outlined by the American Association of Medical Colleges (AAMC) Medical School Objectives Project4 and the Liaison Committee on Medical Education (LCME) in their new standard on knowledge about research principles.5 Our experience is that the anticipation of having to complete these written assignments drives class participation and tends to dictate the content of student questions during class sessions.
From Theory to Practice
There were initial faculty concerns that published cases such as those from the New England Journal of Medicine would be too complex or the discussion too specialized for medical students in the pre-clinical years. However, such misgivings about the concept of the courses are consistently undermined by direct questioning of the students. Further, the vast majority of students agree that reading published papers integrates the curriculum and is an important learning tool.
Our experience confirms Bruner’s hypothesis that “any subject can be taught effectively in some intellectually honest form … at any stage in development.”6 In the past two years, we have successfully read cases of myocardial ischemia after anaphylaxis and of appendicitis with an atypical presentation8 during the first week of medical school (chosen to loosely align with the anatomy course students were taking concurrently, thus allowing for dissections of the chest and abdomen to be coordinated with discussion of the diagnostic approaches to regional pain syndromes).7 Most students can relate from some past experience to the potential seriousness of allergic reactions or to the possible complexities of abdominal pain as a surgical problem. While the detailed information and formal structure of the disciplines relevant to such cases will likely be a long time coming as students progress through the curriculum, it does not preclude having a productive discussion that introduces, at least at an intuitive level, broad medical topics. Consulting a variety of recommended resources while working through these papers, the students are clearly launched into the language and ideas of medicine just a few days after arrival at medical school.
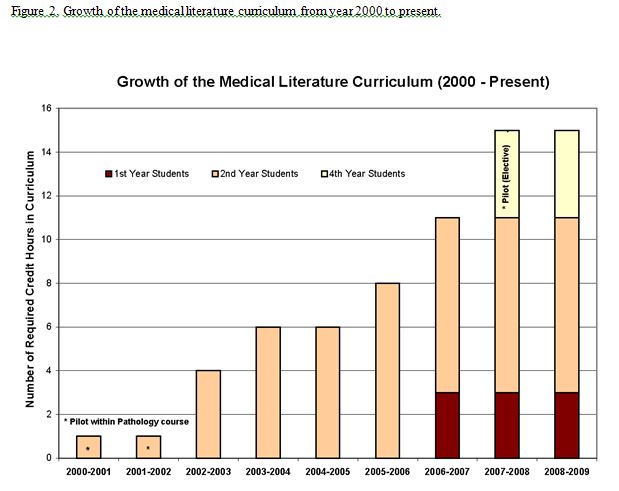
The Medical Literature Curriculum has grown to become a defining educational component of the SUNY Upstate College of Medicine curriculum. The program began as a one-credit case reading supplement encompassed within the second-year pathology course and is currently a 15-credit-hour experience (approximately 9% of the total required credits for graduation) consisting of three longitudinal courses spanning the entire curriculum (illustrated in Figure 2). This growth was gradual and largely the result of student advocacy in curriculum feedback forums in the initial phase and was later bolstered by faculty support and institutional recognition that certain desirable goals and accreditation requirements could be achieved through this mechanism.
In all then, at the present time, our students are required to participate in formal reading of the medical literature
throughout medical school in a longitudinally planned experience that includes careful study of over 50 primary papers representing the entire spectrum of medicine (see website for specific readings) and which has involved participation by faculty from virtually every clinical and basic science department in the school.9 The program takes advantage of the energizing benefits of case study to introduce beginning students to the literature. Later, it offers a mechanism for a return to basic science and for a substantive response to new accreditation standards regarding knowledge of research principles. The Medical Literature Curriculum is designed to model, from the first day of medical school, high-level clinical reasoning, use of basic science knowledge in the discussion of clinical problems and reference to the medical literature as an integral activity of the profession.
Oakeshott (as quoted in Hirst) succinctly captures the overall rationale for this program.10 He says that we are “inheritors … of a conversation … [and] … education is an initiation into the skill and partnership of this conversation.” Further, this conversation consists of an “unrehearsed intellectual adventure” that is increasingly refined over generations and “which, in the end, gives place and character to every human activity and utterance.” We would say that the medical literature represents the conversation of medicine in its most developed and refined form. It is the conversation that we wish our students to engage in now and throughout their careers. As such, it seems reasonable to suggest that we might best promote this by immersing the students in this literature in a formal way throughout medical school under the guidance of the faculty.
ACKNOWLEDGMENTS
The authors wish to thank Professor and Assistant Dean of Curriculum, David Turner, SUNY Upstate, for his continued support of the program and for his wise counsel.
REFERENCES
- Shanley, P.F. Leaving the “empty glass” of problem-based learning behind: new assumptions and a revised model for case study in preclinical medical education. Acad Med. 2007;82(5): 479-85.
- Shanley, P.F., Kelly, K.C. Studying published cases and the medical literature curriculum. Med Educ. 2008;42(5): 521-522.
- Shanley, P.F., Kelly, C. The medical literature curriculum. Med Educ. 2008; 42 (11): 1138-1139.
- Contemporary Issues in Medicine: Basic Science and Clinical Research, American Association of Medical Colleges Medical School Objectives Project Report IV; 2001. http://www.aamc.org/meded/msop/ [Accessed March 15, 2010]
- Current Liaison Committee on Medical Education Accreditation Standards. http://www.lcme.org/standard.htm [Accessed March 15, 2010]
- Bruner, J.S. The Process of Education. Cambridge, MA: Harvard University Press; 1960.
- Jaffe, R., Zahger, D. The domino principle. N Engl J Med. 1996;335(5): 340-341.
- Fisk, D.T., Saint, S., Tierney, L.M. Back to the basics. N Engl J Med. 1999;341(27): 747-750.
- Kelly, K.C., Shanley, P.F. The medical literature curriculum. http://www.upstate.edu/mlc/ [Accessed March 15, 2010]
- Hirst, P.H. Liberal education and the nature of knowledge. In: Knowledge and the Curriculum: A Collection of Philosophical Papers. (pages 30-53). Boston: Routledge & Kegan Paul; 1974.