Abstract
At a regional continuing education conference for pharmacists, 278 attendees answered five questions before and after attending a seminar on important topics in sleep medicine. The purpose of the study was to assess the need for sleep medicine education and to determine the effectiveness of the seminar at the conference. On the pre-test, 80% of the pharmacists answered two or fewer questions correctly. After the seminar, on the post-test, 77% of the pharmacists answered three or more questions correctly. The results of this study indicate that continuing education seminars on sleep medicine are beneficial to pharmacists. In addition, this study provides evidence supporting the need for sleep medicine education in this group of health care professionals.
Introduction
Sleep disorders are highly prevalent, affecting nearly 40 million Americans.1-3 In a national survey, approximately 35% of adults reported disturbed sleep.4 With fatigue and sleep disorders on the rise,5 it is important for health care professionals to understand underlying mechanisms of sleep. One of the primary healthcare professionals on the front line of patient care is the pharmacist.
In American culture, otherwise “healthy” adults with sleep problems are more likely to discuss their sleep disturbances with a pharmacist instead of a physician because of accessibility. Furthermore, some pharmacists perceive sleep aids to be the most misused over-the-counter (OTC) product available.6 Pharmacists are in a unique position to recognize sleep problems7 and to serve as advisors to patients.8 Therefore, sleep medicine education is essential in these health care providers.
Since 1980, when the American Pharmacists Association recognized sleep as a growing problem in the United States,9-10 some continuing education events for pharmacists have included sessions on sleep.11-12 However, to our knowledge, the benefits of such sleep medicine seminars were not assessed. Furthermore, although previous studies have assessed sleep knowledge in nurses, medical students and practicing physicians,13 no study to date, that we are aware of, has assessed sleep knowledge in practicing pharmacists.
The purpose of this study was to demonstrate the benefits of continuing education events featuring sleep medicine education and to substantiate the need for sleep medicine education in the pharmacy curriculum.
Materials and Methods
During a regional conference for Contemporary Issues in Pharmacy, held in Florida, 278 pharmacists from around the state were evaluated on their knowledge of sleep medicine before and after a seminar. The individuals attending the conference were asked to take a pre-test, consisting of five questions, in order to assess their prior knowledge regarding sleep medicine. The pre-test was specifically designed to simulate scenarios attendees may see, or have possibly encountered, as practicing pharmacists.
Description of the Pre-Test
Before the speaker began, each individual was given a No. 2 pencil and one Scantron™ sheet. Participants were told that they should not fill in any identifying information. In this way, the data from the questions would be considered de-identified, thereby protecting the confidentiality of the participants. A projection slide reiterated the instructions. Each question was then projected on the screen. The speaker read each question aloud and asked the participants to choose the best answer from the projected choices (A-E). Sufficient time was given for the participants to read and mark their answer choice. The speaker did not read the answer choices so as not to influence the audience by intonation. Everyone was asked to keep their Scantron™ sheet since they were to be used for a post-test after the seminar. (See Appendix 1 for specific pre-test questions).
Description of the Seminar
The speaker then gave a 45 minute PowerPoint presentation entitled: “The Importance of ‘Good’ Sleep Healthcare for your Patients.” The seminar covered factors that promote “good” sleep, with a particular emphasis on endogenous melatonin, the hormone secreted by the body that induces sleep.1 In addition, various sleep disorders and recent significant sleep research, with potential therapeutic implications, were discussed. The seminar was the final talk of the day, given at 4:00 p.m. on Saturday, May 3, 2003.
The speaker began by defining what constitutes “good” sleep regarding quantity and quality. Individual variations in sleep patterns were examined with regard to age,14-15 gender,16 lifestyle and circadian rhythms.17 Next, the typical endogenous pattern of melatonin secretion was described.18 Emphasis was placed on two principles: 1) melatonin is secreted at night and 2) melatonin secretion is inhibited by bright light.1,19
The point was made that secretion of melatonin is controlled by genetic factors. Therefore, individual variation exists within the population regarding the amount of melatonin secreted and the timing of its secretion. In particular, some individuals are high secretors and some are low secretors. This difference is thought to correlate with heavy and light sleepers, respectively. In addition, the timing of melatonin secretion varies in individuals. Specifically, the rising of melatonin levels earlier in the evening correlates with early birds (advanced phase of secretion). The rising of melatonin levels later in the evening correlates with night owls (delayed phase of secretion). Since genetic factors are involved in the timing of melatonin secretion, time of day preferences for the morning or evening can be seen to run in families. Subsequently, disorders of melatonin secretion, known as circadian rhythms disorders, were described; specifically, Advanced Sleep Phase Syndrome (ASPS)20 and Delayed Sleep Phase Syndrome (DSPS).21 A warning was given to emphasis that DSPS is often misdiagnosed as depression.22 Then treatments for circadian rhythm disorders were outlined.19 Of course, the most effective “treatment” is for a person to maximize their time of day by adapting their lifestyle to fit their sleep-wake cycle. However, since this is not always possible, the most common treatments, utilized by sleep medicine physicians, are bright light therapy and OTC melatonin preparations. 23,24
As an example of how the principles underlying melatonin secretion can benefit individuals, the results from a recent study conducted in night shift workers were presented. The results of the study showed that bright light exposure at night increased performance at work and wearing sunglasses on the drive home improved sleep of the shift workers, presumably by decreasing the inhibition of melatonin secretion.25 In addition, based on recent findings in another study of shift workers, a warning was given that late night meals result in elevated triglycerides.26,27 Factors affecting melatonin levels and sleep, such as caffeine, alcohol and various foods were mentioned.28 Additionally, participants were told of findings from a recent study showing that caffeine, prior to a short nap, will increase performance.29
Jet lag was also discussed with an explanation of the most effective treatments. Emphasis was placed on resetting the body’s internal clock before departure. This can be accomplished by using bright light to shift the sleep-wake schedule. Regarding westward travel, it is thought that delaying sleep a half hour to one hour each night is effective. Regarding eastward travel, OTC melatonin preparations have been found to be effective.28,30
In addition, important research discoveries concerning major sleep disorders were presented. Narcolepsy was described and a warning was given that narcolepsy may be misdiagnosed as insomnia; 50% of narcoleptics report disturbed nocturnal sleep.31,32 Most importantly, the attendees were told of the recent discovery that narcolepsy is associated with a deficiency of the neuropeptide, hypocretin.33 This finding has implications for new therapies such as hypocretin replacement therapy and using hypocretin levels as a diagnostic tool.34
The pharmacists were reminded that OTC melatonin is approved for use in insomnia.35 However, this was quickly followed by a warning that OTC melatonin is contraindicated in patients with a history of depression. This is because OTC melatonin may intensify or exacerbate depression in these individuals.36 Still, there are conflicting views on this point.
To emphasize the importance of sleep medicine research and the potential impact on new pharmacological agents, a recent study in patients with insomnia was presented. The results of the study showed that cerebral blood flow in patients with insomnia was significantly decreased in specific brain regions.37
An overview of topics covered in the seminar is shown below.
Seminar Topics:
•Sleep Hygiene
•Melatonin Secretion
•Circadian Rhythms Disorders
•Melatonin Replacement Therapy
•Bright Light Therapy
•Sleep in Shift Workers
•Effects of Caffeine and Performance
•Restless Legs Syndrome 38-40
•Narcolepsy
•Insomnia
•Jet Lag
Prevalence values for the most common sleep problems were given.4 To emphasize the importance of detecting sleep problems, the effects of sleep problems on everyday life were enumerated.41,42 The pharmacists were reminded that they are on the front-line of healthcare. Therefore, they have the opportunity to make helpful recommendations and have the potential to make a difference in the lives of their clients. A handout with references was included in the course materials booklet for the conference.
Description of the Post -Test
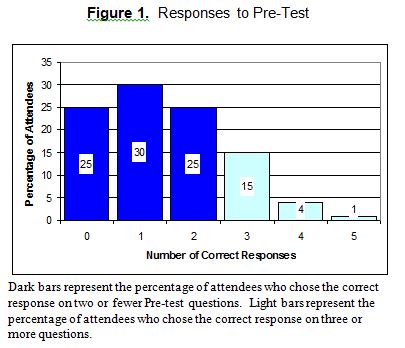
After the seminar, participants took a post-test to assess how much information they retained. The same five questions used in the pre-test were projected and read aloud. The participants were again asked to choose the best answer (A-E). For the post-test, the questions were renumbered 6 through 10. In addition, since the attendees would be using the same Scantron™ sheet they used for the pre-test, the answer choices on the post-test were rearranged. This was done to discourage anyone from changing their answers on the pre-test questions. (See Appendix 2 for specific post-test questions.)
RESULTS
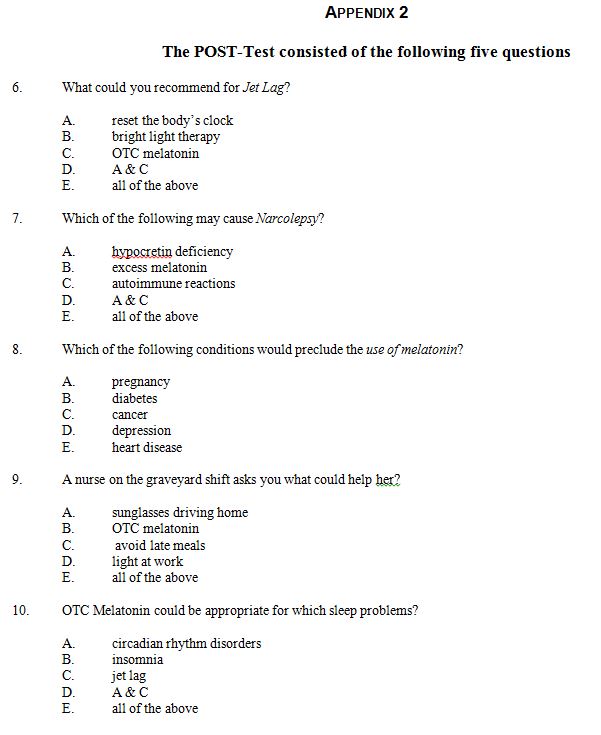
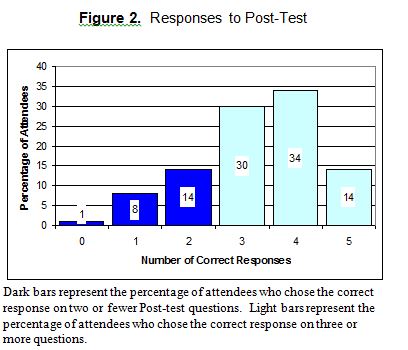
The results of the pre-test and post-test are summarized in Tables 1 and 2 respectively. The results of the pre-test and post-test are graphically represented in Figures 1 and 2 respectively. On pre-test question one, a large number of the attendees responded that for jet lag they would recommend OTC melatonin (31%) or reset the body’s clock (30%). However, after the seminar, on the post-test, the responses to question six showed that the majority of the attendees (44%) learned that both OTC melatonin as well as resetting the body’s clock could be recommended for jet lag. In addition, a significant portion (33%) of the audience remembered that the body’s clock can be reset by bright light exposure and therefore would be helpful for jet lag. When added together, the attendees who selected the correct answer (E = 33%) and those who chose the next best answer (D = 44%), the results show that 77% of the attendees retained the major points of the seminar.
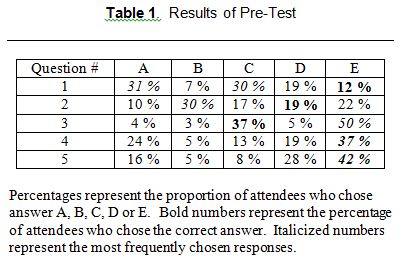
On pre-test question two, a large number of the attendees (30%) thought that narcolepsy was caused by excess melatonin. However, after the seminar on the post-test, the responses to question seven showed that many of the attendees learned that narcolepsy is caused by hypocretin deficiency (37%). Furthermore, a large number of the attendees learned that narcolepsy is also associated with autoimmune reactions (45%). Similarly to the first question above, when added together, the attendees who selected the correct answer (D=45%) and those who chose the next best answer (A=37%), the results show that a remarkable majority of the attendees (82%) retained the major points of the seminar.
On pre-test question three, a large number of the attendees thought that pregnancy would preclude the use of melatonin (50%). A significant number knew that depression would preclude the use of melatonin (37%). However, after the seminar on the post-test, the responses to question eight show that almost all of the pharmacists (96%) recognized that depression was the most serious condition that would preclude the use of melatonin.
On pre-test question four, a large number of the pharmacists (37%) recognized the major things that would be helpful to a nurse working the graveyard shift. However, a significant number of the attendees only recognized OTC melatonin as a potential benefit (24%). But after the seminar on the post-test, the responses to question nine showed that an overwhelming majority (83%) of the attendees were able to recognize the major things that would be beneficial to a night shift worker, such as a nurse on the graveyard shift.
On pre-test question five, a large number of the attendees (42%) recognized major sleep problems that would benefit from OTC melatonin. However, a substantial number of attendees, indicated by the percentage of responses for On pre-test question five, a large number of the attendees (42%) recognized major sleep problems that would benefit from OTC melatonin. However, a substantial number of attendees, indicated by the percentage of responses for choices A and D, were unaware that melatonin is used to treat circadian rhythms disorders or they were unfamiliar with these types of sleep disorders. However, after the seminar on the post-test, the responses to question ten show that there was an increase in the number of individuals who understood that melatonin would be appropriate to treat these sleep problems. Ironically, 17% of the attendees failed to recognize that melatonin could be used for insomnia. However, added together, the results indicate that the majority of the attendees (84%) retained the major points of the lecture.
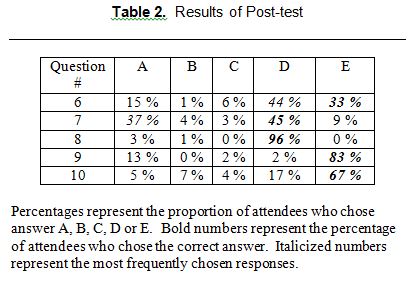
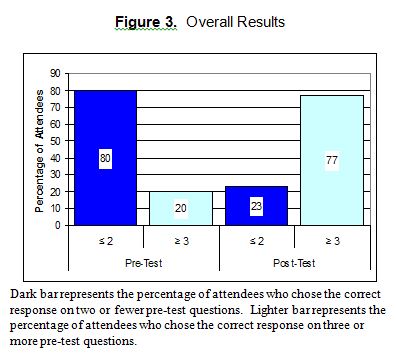
On the pre-test, nearly 80% of the participants answered only two or fewer questions correctly (Figures 1 & 3). In contrast, after the seminar, 47% of the participants answered four or five questions correctly and 77% answered three or more questions correctly (Figures 2 & 3). Even individuals having no correct responses on the pre-test significantly improved their knowledge of sleep medicine with 63% of these participants having two or three correct responses on the post-test. Furthermore, a comparison of correct responses between the pre-test and the post-test reveals a significant increase in the percentage of correct responses on the post-test. In addition, the format of the questions allowed the examiners to differentiate between individuals who retained the maximal information and those who mastered the major points, but missed the minor ones. Unfortunately, due to the limited number of questions, the test reliability number was low for the pre-test (0.40) as well as the post-test (0.39).
DISCUSSION
Although the amount of medical knowledge has increased exponentially, the medical curriculum has been unable to expand proportionally. Unfortunately, due to the time constraints of the medical curriculum, physicians are poorly trained in the area of sleep medicine.43,44 Therefore, even individuals who voice their sleep complaints to their physicians are often misdiagnosed with depression and anxiety disorders.22
Similarly, topics pertaining to sleep medicine are minimal or dispersed throughout the pharmacy curriculum. For example, although the biosynthetic pathway of melatonin is usually covered in biochemistry, the pattern of melatonin secretion and its effect on sleep patterns is not discussed.45 Also, time constraints in the general physiology course may preclude the discussion of the basic physiology of sleep.46 Often, the extent of their training leaves the future pharmacist with only one doctrine: “melatonin induces sleep”. The particulars of how and when this important hormone works are usually not covered.
The results of our study suggest that practicing pharmacists have had little exposure to sleep medicine education. The findings on the pre-test suggest that training in the area of sleep medicine is essential. The responses on the post-test indicate that the majority of the attendees were able to assimilate the major points from the lecture. In addition, the percentage of individuals who responded correctly to questions one and two on the post-test showed their ability to grasp the big picture, as well as sub points. Therefore, our study indicates that sessions on sleep medicine, similar to the one in our study, would be beneficial for practicing pharmacists. Furthermore, with the explosion of data being published in the field of sleep research, it is imperative that the topic of sleep be expanded in the pharmacy curriculum.
Although pharmacists are unable to diagnose sleep disorders, a basic understanding of sleep patterns and circadian rhythms is crucial. Knowledge of the body’s melatonin secretion pattern would enable pharmacists to better advise their clients regarding their sleep problems. In particular, an understanding of the endogenous secretion of melatonin, and its possible individual variations would be extremely helpful when they discuss OTC melatonin preparations with their clients.
For example, night owls may be interested in taking melatonin to go to sleep earlier. The melatonin secretion in these individuals typically rises later at night. On the other hand, early birds may be interested in taking melatonin to go back to sleep because they arise earlier in the morning. The melatonin secretion in these individuals typically rises earlier in the evening and declines early in the morning.
Furthermore, melatonin secretion varies with age. Teenagers, for example tend to be night owls because their rise in melatonin secretion occurs later at night.47 For this reason, studies are being conducted to reevaluate school start times.48 In addition, melatonin secretion declines with age31. Therefore, melatonin replacement therapy may be beneficial in the elderly.49
More training will give pharmacists a better understanding of sleep and enable them to appropriately answer questions regarding OTC melatonin preparations and refer clients to sleep clinics when necessary.9 With a focus today on promoting wellness, the importance of sleep should move to the forefront of healthcare. More importantly, over the past century, changes in lifestyle have made an understanding of factors promoting good sleep essential. Today there are more double-income families than ever before. Yet, the stressors in our daily lives have increased substantially. Therefore, being in “good” health is a matter of survival. By extension, a good night’s sleep is one of the fundamental elements of good health. With over one-third of Americans complaining of disrupted sleep, it is essential that health care professionals be better trained in this area.
Various sleep medicine organizations have made efforts to educate physicians as well as the general public. For example, the National Sleep Foundation (NSF), in conjunction with the Sleep Research Society (SRS) will be hosting a conference at the NIH on March 29 & 30, 2004 (http://www.nhlbi.nih.gov/meetings/slp_front.htm). The American Academy of Sleep Medicine (AASM) has a series of excellent brochures which are aimed at patient education. Most recently, the pharmacy profession has begun to utilize online methods to provide continuing pharmaceutical education. An example of this type of article, focusing on insomnia, the sleep cycle and treatments, can be found at this website (http:// secure.pharmacytimes.com/lessons/200306-01.asp). However, health care professionals must be made aware of these resources. For the practicing pharmacist, this could be accomplished with seminars, such as the one described in our study or through online continuing education endeavors as described above. Currently medical educators interested in sleep medicine education are working to develop a plan to integrate sleep topics into the medical school curriculum.50 Hopefully in the future, the pharmacy curriculum will also be expanded to cover sleep medicine in more detail.
CONCLUSIONS
The design of the present study allowed the assessment of the baseline level of knowledge of sleep medicine in practicing pharmacists. The results of the pre-test indicate that prior knowledge of sleep medicine regarding melatonin was minimal and that sleep medicine education is needed. The results of the post-test showed that the majority of the conference attendees significantly improved their knowledge of sleep medicine by attending the seminar. In addition, the results of this study indicate that presentation of the material in a lecture format was an effective way of increasing the knowledge level of the attendees, regardless of their individual educational backgrounds. We hope the results of this study provide an impetus to include sleep medicine education as part of continuing educational events for pharmacists, and eventually as part of the pharmacy curriculum.
REFERENCES
- Turek FW. Chronobiology. In: Principles and Practice of Sleep Medicine. Kryger MH, Roth T, Dement WC eds. Philadelphia: Saunders, 3rd ed. 2000; p. 319-400.
- Broman JE, Lundh LG, Hetta J. Insufficient sleep in the general population. Neurophysiologie Clinique 1996; 26(1): 30-9.
- Kuppermann M, Lubeck DP, Mazonson PD, Patrick DL, Stewart, AL, Buesching DP, Fifer SK. Sleep problems and their correlates in a working population. Journal of General Internal Medicine 1995; 10(1): 25-32.
- Zamarron C, Gude F, Otero Y, Alvarez JM, Golpe A, Rodriguez JR. Prevalence of sleep disordered breathing and sleep apnea in 50-70 year-old individuals. A survey. Respiration 1999 66(4): 317-22.
- Searle Sleep disorders create growing opportunities for hospitals. Health Care Strategic Management 2001; 19(2): 16.
- Akram G, Mason R, Millson D, Blenkinsopp A. Determining the feasibility of pharmacy based research using over-the-counter (OTC) sleep aids as a model. Health Services Research & Pharmacy Practice 2000; Abstracts: 22.
- Wincor MZ. The pharmacist’s role in the recognition and management of insomnia. Journal of Clinical Psychiatry 1992; 53(S80-3).
- Linn LS, Davis MS Occupational orientation and overt behavior – the pharmacist as drug advisor to patients. American Journal of Public Health 1973; 63(3):502-8.
- Kennedy JS Awakening the nation to sleep problems. American Pharmacy 1980; NS20(12):24.
- Welch JS APhA joins “Project Sleep”. American Pharmacy 1980; NS20(4):10-1.
- The College of Psychiatric and Neurologic Pharmacists Annual Meeting. Charleston, South Carolina (May 1-4, 2003)
- 9th Annual Neuropsychiatric Pharmacology Update. University of Arizona, College of Pharmacy, Health Science Center Phoenix (October 16 & 17, 2003)
- Zozula R, Bodow M, Yatcilla D, Cody R, Rosen RC Development of a Brief, Self-Administered Instrument for Assessing Sleep Knowledge in Medical Education: “The ASKME Survey”. Sleep 2001; 24(2): 227-233.
- Haimov I, Laudon M, Zisapel N, et al. Sleep disorders and melatonin rhythms in elderly people. British Medical Journal 1994; 309:167.
- Baskett JJ, Arendt J, et al. Does melatonin improve sleep in older people? Age and Ageing 2003; 32(2): 164-170.
- Murphy PJ, DeMatteo MK, Campbell SS. Sex hormones and sleep in postmenopausal women: estrogen/LH balance and sleep quality. Sleep 2000; 23(S2):A126.
- Arendt, J. Importance and relevance of melatonin to human biological rhythms. Journal of Neuroendocrinology 2003; 15(4): 427-431.
- Dawson D, Encel N. Melatonin and Sleep in Humans. Journal of Pineal Research 1993; 15:1-12.
- Hughes RJ, Lewy AJ. Light and melatonin treatment of circadian phase sleep disorders. In: Lam RW, ed. Seasonal Affective Disorder and Beyond: Light Treatment for SAD and Non-SAD conditions. American Psychiatric Press: Washington, D.C.; 1998; p.221-252.
- Jones CR, Campbell SS, Zone SE, et al. Familial advanced sleep phase syndrome: a short-period circadian rhythm variant in humans. Nature Medicine 1999; 5:1062-5.
- Archer SN, Robilliard DL, Skene DJ, Smits M, Williams A, Arendt A, von Schantz M. A length polymorphism in the circadian clock gene Per3 is linked to delayed sleep phase syndrome and extreme diurnal preference. Sleep 2003; 26(4): 413-415.
- Zee P. Circadian rhythm sleep disorders. Program for the Eighth Meeting of the Society for Research on Biological Rhythms (May 21-26, 2002), p. 7.
- Lewy AJ, Wehr TA, Goodwin FK. Light suppresses melatonin secretion in humans. Science 1980; December p.210.
- Dahlitz M, Alvarez B, Vignau J, et al. Delayed Sleep Phase Syndrome response to melatonin. Lancet 1991; 337: 1121-1124.
- In-Young Yoon, et al. Bright light exposure at night and light attenuation in the morning improve adaptation of night shift workers. Sleep 2002; 25(3): 351-356.
- Arendt J. Shift-work: adapting to life in a new millennium. Program for the Eighth Meeting of the Society for Research on Biological Rhythms (May 21-26, 2002), p. 7.
- Sopowski MJ, Hampton SM, Ribeiro DC, Morgan L, Arendt J. Post-prandial triacylglycerol responses in simulated night and day shift: gender differences. Journal of Biological Rhythms 2001; 16 (3): 272-276.
- Reiter RJ. Creating a Melatonin-Friendly Lifestyle and Back in Sync. In: Reiter RJ, Robinson J. eds. Melatonin. New York, NY: Bantam Books 1995; p.110-199.
- Van Dongen HP. The effect of caffeine and naps on performance. Program for Sleep Symposium 2000. Glade Springs, WV (October 22, 2000).
- Arendt J, Aldhous M, English J, et al. Some effects of jet lag and their alleviation by melatonin. Ergonomics 1987; 30:1379-1393.
- Schmidt H. Narcolepsy and sleep disordered breathing. Program for the 9th Annual Keynote Symposium: Sleep Medicine 2000. Dublin, Ohio (September 29, 2000) hosted by the Ohio Sleep Medicine Institute.
- Parkes JD, Chen SY, Clift SJ, Dahlitz MJ, Dunn G. The clinical diagnosis of the narcoleptic syndrome. Journal of Sleep Research 1998; 7(1): 41-52.
- Peyron C, Mignot E, et al. A mutation in a case of early onset narcolepsy and a generalized absence of hypocretin peptides in human narcoleptic brains. Nature Medicine 2000; 6 (9): 991-997.
- Kanbayashi T, et al. Hypocretin-1 (Orexin-A) levels in human lumbar CSF in different age groups: infants to elderly persons.” Sleep 2002; 25(3): 337-339.
- Ellis CM, Lemmens G, Parkes JD. Melatonin and insomnia. Journal of Sleep Research 1996; 5:61-65.
- Kripke DF. Melatonin in aging depressives. Program for Eighth Meeting of the Society for Research on Biological Rhythms. Amelia Island, FL (May 21-26, 2002), p.23.
- Smith MT, Perlis ML, Chengazi VU, Pennington J, Soeffing J, Ryan JM, Giles DE. Neuroimaging of NREM Sleep in Primary Insomnia: A Tc-99-HMPAO Single Photon Emission Computed Tomography Study. . Sleep 2002; 25(3): 325-335.
- Ekbom KA. Restless legs. Acta Medica Scandinavica Supplementum 1945; 158:1-123.
- Phillips B, Young T, Finn L, Asher K, Hening WA, Purvis CC. Epidemiology of Restless Legs Syndrome in adults. Archives of Internal Medicine 2000; 160:2137 – 2141.
- Early C, Connors JR, Allen RP. RLS patients have abnormally reduced CSF ferritin compared to normal controls. Neurology 1999; 52: Alll-112.
- Kapur V, Redline S, Nieto J, Young T, Newman AB, Henderson JA. The relationship between chronically disrupted sleep and healthcare use. Sleep 2002; 25(3):289-296.
- Baldwin CM, Griffith KA, Nieto J, O’Connor GT, Walsleben JA, Redline S. The association of sleep-disordered breathing and sleep symptoms with quality of life in the sleep heart health study. Sleep 2001; 24(1): 96-105.
- Rosen RC, et al. Low rates of recognition of sleep disorders in primary care: comparison of a community-based versus clinical academic setting. Sleep Medicine 2001; 2(1):47-55.
- Orr, W.C. Physician Education in Sleep Disorders. Journal of Medical Education 1980; 55(4): 367-69.
- Personal communication with Dr. V.K. Venkatachalam, Associate Professor of Biochemistry who teaches for the NSU College of Pharmacy
- Personal communication with Dr. David King, Assistant Professor of Physiology who teaches at NSU College of Pharmacy
- Cavallo A. Melatonin and human puberty: current perspectives. Journal of Pineal Research 1993; 15:115-21.
- Dexter D, Bijwadia J, Schilling D, Applebaugh G. Sleep, sleepiness and school start times: a preliminary study. Wisconsin Medical Journal: the official publication of the State Medical Society of Wisconsin. 2003; 102(1): 44-6.
- Garfinkel D, Laudon M, Nof D, et al. Improvement of sleep quality in elderly people by controlled-release melatonin. Lancet 1995; 346: 541-544.
- Harding SM, Berner ES. Developing an action plan for integrating sleep topics into the medical school curriculum. Sleep Breath 2002; 6(4):155-60.
APPENDIX 1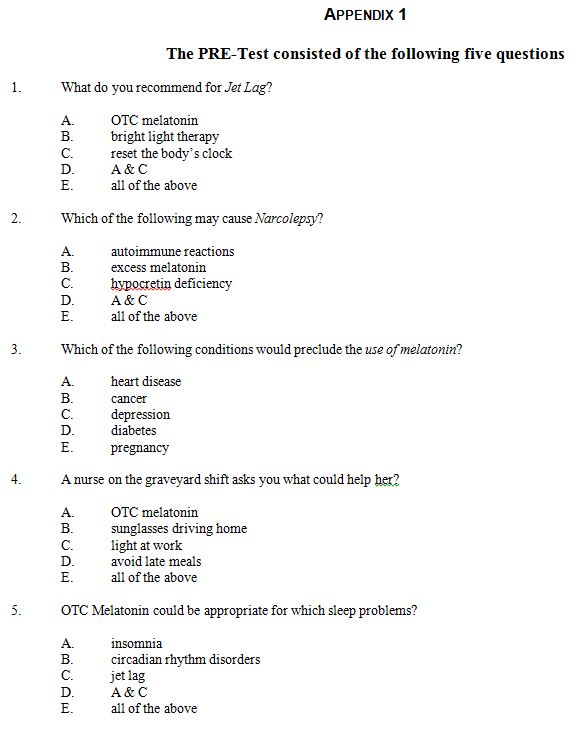
APPENDIX 2