ABSTRACT
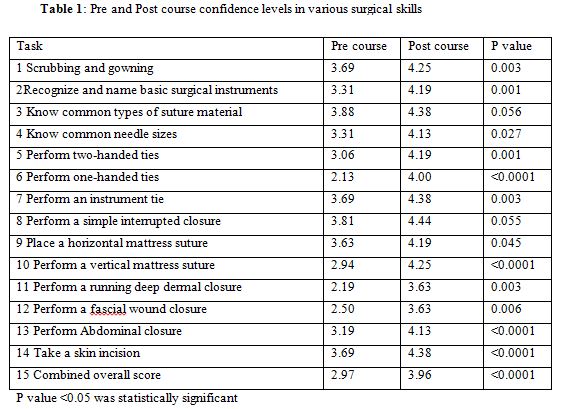
Surgical skills training plays an important role in residency training. The training and development of technical skills have largely been confined to the operating room. Although most institutions in the West have implemented surgical skills training programs for surgical residents, few such programs exist in India. A basic surgical skills course was conducted for surgical residents in liaison with ETHICON Institute of Surgical Education. Sixteen students were enrolled in the course. The course consisted of a short lecture followed by hands on instruction and practice. The students were allowed to spend additional time practicing and refining the skills that were taught. The course was divided into six sessions: 1) overview of suture material, 2) handling of surgical instruments, 3) sutures and needles, 4) basic suturing techniques and 5) opening and closing of abdomen. The students were provided with the surgical instruments, suture material, knot tying board and a suturing pad to practice knot tying. A pre course versus post course survey of the students’ perceived self assessment score for all the skills combined rose from 2.97+0.6 to 3.96+0.3 (p value < 0.0001).The students thought the course was highly relevant to their current level of training (mean rating 4.8+0.5) and comfort levels performing the skills taught compared with before the course was markedly improved (4.5+0.6).
Since knowledge of surgical skills is becoming increasingly important, these results are presented to the curriculum committee to consider integrating the surgical skills course into the first year of postgraduate curriculum. The earlier in one’s career that proper suturing and knot tying technique is learned, the more opportunity there will be for practice and development of the speed, efficiency and precision that is characteristic of expert performers.
There is good evidence that procedural simulation improves operational performance in actual clinical settings.1 The training and development of technical skills has largely been performed in the operating room. Although most institutions in the West and Tanzania under low resource settings have implemented surgical skills training program for surgical residents, few such programs exist in India.2 In the current model of surgical training, based primarily on apprenticeship, the opportunities for deliberate practice are rare. Operations are complex, and it is difficult to focus on one small component of the procedure.3 A needs assessment survey of advanced surgical trainees at this hospital demonstrated that skills were usually acquired during sessions in the operating theatre often in an ad hoc manner. They felt the need of more practical training by the faculty in a form of workshop. We report our experience in establishing a workshop-based skills course which was conducted for first year surgical residents in liaison with ETHICON Institute of Surgical Education.
Sixteen post graduate students were enrolled in the course. The course consisted of a short lecture followed by hands on instruction and practice. The course was divided into five sessions: 1) overview of suture material, 2) handling of surgical instruments, 3) sutures and needles, 4) basic suturing techniques and 5) opening and closing of abdomen. Students were provided with the instruments, suture material, knot tying board and a suturing pad to practice trying knots. Students were allowed to spend additional time practicing and refining the skills that were taught. The students completed pre- and post-training questionnaires to measure self-perceived confidence in performing select surgical procedures. Students rated their confidence on a five-point Likert scale, (1) “Very unconfident” to (5) “Very confident”. The post-training survey also included qualitative questions on how the training changed student perception of practicing surgery as well as recommendations for improvement of the training. Descriptive statistics for the items on the survey including percentages, means and standard deviations were calculated. Matched paired t-tests were used to compare pre course to post course confidence levels of students using SPSS version 17 software.
The study was approved by Kamineni Institute of Medical Sciences Institutional Research Committee.
The pre-course versus post -course survey of student-generated self assessment score for all the skills combined rose from 2.97+0.6 to 3.96+0.3(p value < 0.0001). [Table 1] The students thought the course was highly relevant to their current level of training (mean rating 4.8+0.5) and comfort levels for performing the skills taught, when compared to before the course, was markedly improved (4.5+0.6). There was overall satisfaction with the manner in which the skills were taught (hands-on apprenticeship with oral guidance) and the individual attention each student received to learn the skills. The simulation for abdominal opening and closure included a balloon placed beneath the abdominal wall and the participant should be able to open and close abdomen without bursting the balloon. All the participants could not perform the procedure initially but after the session on abdominal closure, thirteen out of sixteen participants could do the procedure. Ninety one percent of the respondents strongly agreed that the training was a valuable use of their break time, believed it would help them provide better patient care and would recommend the training to their juniors. Students reported an increase in willingness and preparedness to carry out surgery after the training. Comments from participants included: ‘Improvement themes related to wanting longer duration of training and broadening of the skills covered to include procedures such as endotracheal intubation and chest tube insertion’. One participant felt ‘I could learn how to hold the knife in a proper way today’. Participants also requested for the suturing pad and other materials to be taken home so that they can practice.
A major advantage of a course of this nature for relative surgical “novices” is that the skills are taught by experts in a low-key, non pressurized environment rather than in the operating room, where time pressures and patient safety are paramount. Since there was no formal surgical skill training being offered for the surgical residents, we tried to see if the residents would benefit from such training. The participants were initially not able to perform the skills taught in a methodical manner: for example one of the participants was touching the gown with bare hands when putting on the gown and one participant was touching the fingers of the gloves while donning the gloves. All the participants were asked to perform the skills taught before teaching and were then shown the proper way to be followed on a one to one basis, since we had time in a low key, non pressurized environment. It would not be possible to teach the suturing in the theatre on the patient while the patient anesthesia time keeps on increasing. Six out of sixteen participants felt the need for more time in teaching deep dermal closure. Ericsson and others have pointed out that learning is enhanced in low-tension environments, but high-level tension, such as is often found in the operating room, inhibits learning of motor skills because of associated anxiety.4,5
Surgical skills are becoming increasingly important in surgical education. The findings of the study have been reported to the curriculum committee for them to consider integrating the surgical skills course into the first year of postgraduate curriculum beginning with the next academic year. In the future, the improvement in the time taken and the precision of performing the suturing will be assessed. The earlier in one’s career that proper suturing and knot tying technique are learned, the more the opportunity will be for practice and development of the speed, efficiency and precision that is characteristic of expert performers. The major advantage of the course is that skills are being taught by experts in a low-key, non pressurized environment rather than in the operating room. Medical colleges and universities should consider integrating a surgical skills course into the first year postgraduate curriculum.
Competing Interests: The authors declare that they have no competing interests.
Sources of funding: Kamineni Institute of Medical Sciences research grant and Ethicon institute.
ACKNOWLEDGEMENTS
The authors would like to thank Col. Dr C.G. Wilson Principal, Kamineni Institute of Medical Sciences for his support and encouragement and for permitting us to initiate this curriculum change. Our sincere thanks to faculty members for their help and post graduates for their active participation. Our special thanks to the management of Kamineni Institute of Medical Sciences for the encouragement. We would like to thank Ethicon institute for providing the material required for the course.
REFERENCES
- Nishisaki, A., Keren, R., and Nadkarni V. Does simulation improve patient safety? Self-efficacy, competence, operational performance, and patient safety. Anesthesiology Clin. 2007; 25: 225–236.
- Tache ,S., Mbembati, N., Marshall, N., Tendick, F., Mkony, C., and O’Sullivan, P. Addressing gaps in surgical skills training by means of low-cost simulation at Muhimbili University in Tanzania. Human Res. for Health. 2009; 27 {7}: 64.
- Reznick, R.K., and MacRae, H. Teaching surgical skills changes in the wind. New Eng. J. Medicine. 2006; 355: 2664-2669.
- Ericsson, K.A. The acquisition of expert performance: an introduction to some of the issues. In: The road to excellence: the acquisition of expert performance in the arts and sciences sports and games. Mahwah, N.J. Lawrence Erlbaum, 1996; 1–50.
- Pellegrini, C.A. Surgical education in the United States: navigating the white waters. Ann. Surgery. 2006; 244: 335–342.