ABSTRACT
This study explores medical student attitudes on the effectiveness of Team-Based Learning (TBL) after completing their first year in a TBL curriculum. While individual attitudes toward many aspects of TBL varied, our data suggest that TBL is seen as an effective tool for use in supplementing medical education.
Large class sizes, compromised faculty time, and an ever-expanding knowledge base have made didactic lectures the instrument of choice for many medical educators.1 However, medical school faculty have long recognized the importance of clinical application, group problem solving, and active learning in preparing first and second year medical students for national board examinations and clinical clerkships. Indeed, since the American Association of Medical Colleges (AAMC) first recommended that a problem-based, student-centered curriculum emphasizing the integration of basic and clinical sciences should be an essential component of pre-clinical medical education, medical educators have struggled to find effective teaching methods which actively engage students in the learning process.2 While numerous strategies have evolved to supplement didactic lectures with active learning, a paucity of information exists within the literature regarding medical student attitudes toward the effectiveness of such active learning methods.
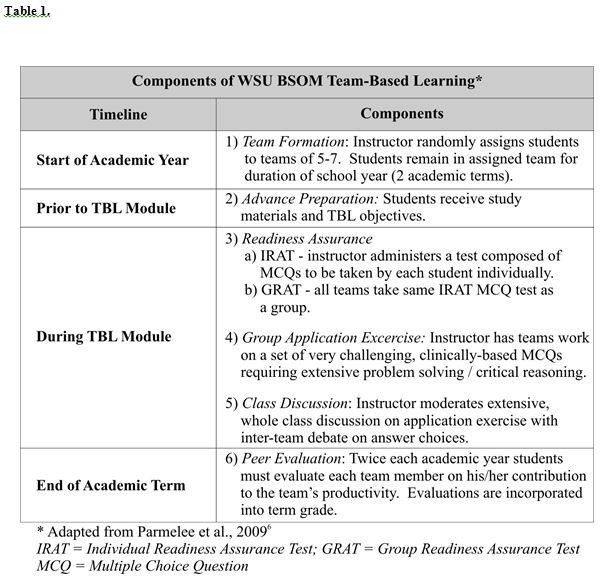
Team-Based Learning (TBL) is a well-defined instructional strategy, first developed for large business school classes, that is being increasingly employed in medical education.3-5 It requires small groups to work together to solve problems in an instructor-led but learner-centered environment with well-structured processes of individual and group accountability (Table 1).6 In 2002, TBL was introduced as a supplemental educational strategy into Wright State University Boonshoft School of Medicine’s (WSU BSOM) predominately lecture-based preclinical curriculum. Since then, the school has been at the forefront in utilizing this innovative form of authentic assessment along with discipline- (year 1) and system-based (year 2) didactic lectures. It has created an active learning environment that promotes both mastery of the facts of course content as well as application of course concepts to solving complex clinical problems. In distinct contrast to Problem-Based Learning (PBL), the strategy involves one to three faculty for a session conducted entirely in one room.
Numerous studies have shown that TBL incorporates effective small-group learning into large group lecture-oriented classes, thereby increasing student participation, preparedness, communication, teamwork skills, and knowledge outcomes.1,5,7-9 However, it is critical that one not underestimate the importance of student confidence in judging the worthiness of any active learning experience.10 Pre-clinical students frequently feel overwhelmed by the amount of information they must acquire through individual study, sometimes resulting in skepticism toward active learning exercises that require large investments of time in exchange for questionable gains in factual knowledge.1 Often, in spite of the fact that active learning methods incorporate and/or prepare students for course specific summative testing (ex: IRAT/GRAT, Final Examinations), students instead prefer the safety and assurance inherent in an efficiently taught lecture covering only information pertinent for national board examinations and “real life” medical situations. The specific aims of the current study were to ascertain student perspectives regarding the effectiveness of TBL compared to other active learning strategies in fostering critical reasoning and clinical problem solving skills and determine which aspects of TBL are particularly effective or ineffective at promoting retention of course material as indicated by subjective student experience on exam performance.
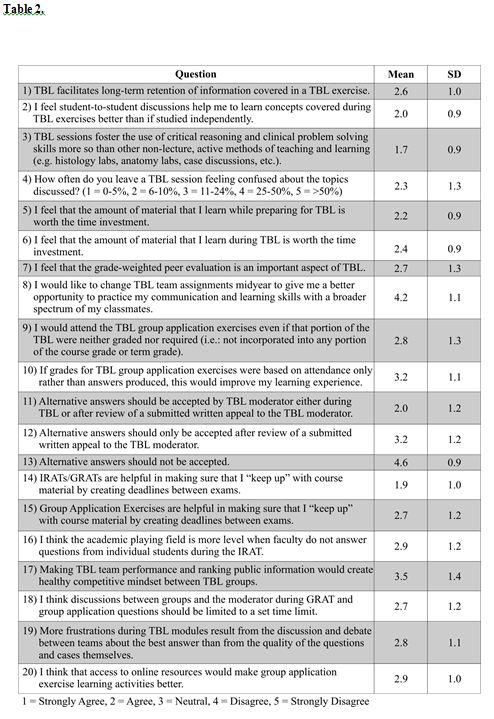
With institutional review board approval, the 2008-2009 first year class at the Wright State University Boonshoft School of Medicine participated in this study. In a classroom setting at the end of their first year in a medical school curriculum supplemented by TBL, laboratory exercises, case discussions, and “audience response” lectures, students anonymously completed a 20-item Likert Questionnaire (1 = Strongly Agree, 2 = Agree, 3 = Neutral, 4 = Disagree, 5 = Strongly Disagree) with 2 “write-in” prompts to assess attitudes toward different aspects of TBL compared with other active learning educational strategies. The survey, developed after a thorough literature review to assess intended outcomes of TBL, was approved by WSU BSOM course directors and TBL moderators. The questionnaire took approximately 15 minutes to complete. Response rates were 100% (n=94) for Likert questions, 38.3% (n=36) for write-in prompt 1 and 48.9% (n=46) for write-in prompt 2.
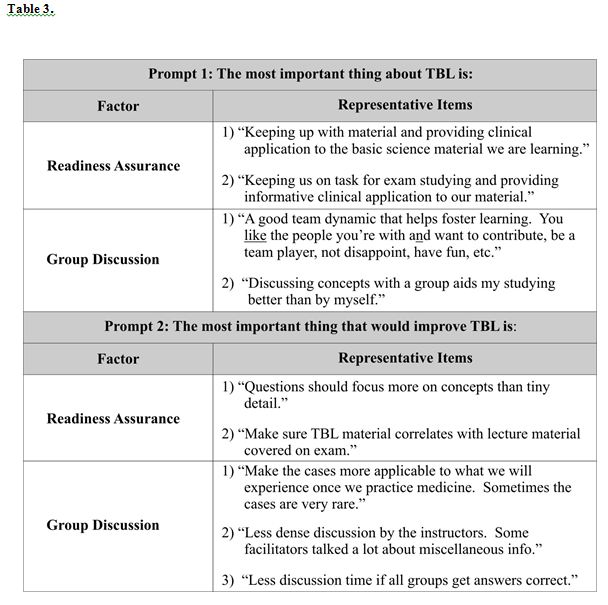
The preponderance of student responses in the “neutral” range of the Likert scale indicates there is a great deal of variability among student attitudes regarding various aspects of TBL. However, several trends are apparent within the data. Of students polled, 82.9% reported that they “agree” or “strongly agree” with the statement that readiness assurance testing creates manageable deadlines between course examinations (Table 2 Question 14; Table 3). By fostering advanced preparation, TBL helps students who may be less intrinsically motivated to properly structure their study time. Accordingly, 65.9% of students reported they “agree” or “strongly agree” that preparing for TBL is an effective use of study time (Table 2 Question 5; Table 3). It further appears that intellectual gains fostered through TBL extend beyond the mere act of preparing for and taking readiness assurance tests. Our data suggest that a majority of students view the time spent in TBL as a worthwhile learning experience (Table 2 Question 6). Indeed, if this were not the case, periodic individual multiple choice quizzes could replace TBL. It should be noted, however, that data from written responses indicate the process may be more effective with an increased basis on conceptual lecture materials as well as making the clinical cases more applicable to the daily practice of medicine (Table 3).
By allowing for directed small group discussion among peers, 77.7% of students reported they “agree” or “strongly agree” that concepts covered during TBL are more effectively learned than through independent study alone (Table 2 Question 2; Table 3). It is within group discussion that many have postulated the benefits of TBL are uncovered.1,9 Particularly for struggling students, it may be that the mutual consensus of ideas amongst team members necessary to reach a unified response on Group Readiness Assurance Tests and Application Exercise problems provides productive feedback as well as better retention of knowledge.1,9 In concordance with such posits, 84.0% of students responded that they “agree” or “strongly agree” that TBL fosters the use of critical reasoning and clinical problem solving more so than other active methods of teaching and learning (Table 2 Question 3). Further evidence suggesting the importance of team discussion can be found in the written responses, where some students indicated that too much discussion by the instructor can become counterproductive (Table 3). However, when presented with the option of time limits during team discussion, student opinion varied, indicating that group discussion is of paramount importance (Table 2 Question 18). The acquisition and gradual mastery of such skills within a group promotes healthy team dynamics and a strong sense of team unity, as evidenced by the 71.3% of students who reported that they “disagree” or “strongly disagree” that a mid-year change in TBL team assignments would help people further build teamwork skills (Table 2 Question 8; Table 3).
TBL is an education strategy designed to develop higher order cognitive skills students can apply to real world, clinical problems. By creating a learning environment that depends upon productive group interaction and individual accountability of team members, it prepares students for the clinical experiences which rely heavily on teamwork skills, critical thinking, and problem solving. While individual attitudes toward many aspects of TBL may vary, our data suggest that first year medical students see TBL as a more effective opportunity to foster critical reasoning and clinical problem solving skills than other non-lecture, active methods of teaching and learning (ex: labs and case discussions), as well as allowing for enhanced learning of core concepts through student to student interaction. It is our opinion that, because students view this authentic assessment strategy not merely as assessment, but as learning, it can be applied effectively in a medical school setting. Findings should be interpreted, however, in light of the study’s limitation that responses are from one class of medical school students. Future studies should include the progression of student attitudes toward TBL over a prolonged time period.
ACKNOWLEDGEMENTS
We wish to sincerely thank Dr. John F. Donnelly, M.D., Dr. B. Laurel Elder, Ph.D., Dr. Paul G. Koles, M.D., Dr. Gary L. Neider, Ph.D., Dr. Gary M. Onady, Ph.D., and Dr. Larry J. Ream, Ph.D. for providing feedback on survey development and for their support of this project. Their devotion to students has been an inspiration.
REFERENCES
- Koles, P., Nelson, S., Stolfi, A., Parmelee, D., DeStephen, D. Active learning in a Year 2 pathology curriculum. Med Educ 2005; 39: 1045–1055.
- Muller, S. Physicians for the twenty-first century: Report of the project panel on general professional education of the physician and college preparation for medicine. J Med Educ 1984; 59:1-208.
- Michealson, L.K., Watson, W.E., Cragin, J.P., Fink, L.D., Team Learning: A potential solution to the problems of large group classes. Exchange: The Organizational Behavior Teaching Journal 1982; 7:13-22.
- Michaelsen, L.K., Fink, L.D., Knight, A. Designing effective group activities: lessons for classroom teaching and faculty development. In: DeZure D, editor. To improve the academy: resources for faculty, instructional and organizational development. Vol. 17. Stillwater, OK: New Forums Press. 1997.
- Thompson, B.M., Schneider V.F., Haidet, P., Levine, R.E., McMahon, K.K., Perkoski, L.C., Richards, B.F. TBL at ten medical schools: two years later. Med Educ 2007; 41: 250–257.
- Parmelee, D.X., DeStephen, D., Borges, N.J. Medical students attitudes about TBL in a Pre-Clinical Curriculum. Med Educ Online 2009; 14:1
- Vasan, N.S., DeFouw, D.O., Compton, S. A survey of student perceptions of TBL in anatomy curriculum: Favorable views unrelated to grades. Anat Sci Educ 2009; 2: 150-155.
- Levine, R.E., O’Boyle, M., Haidet, P., Lynn, D.J., Stone, M.M., Wolf, D.V., Paniagua, F.A. Transforming a clinical clerkship through team learning. Teach Learn Med 2004; 16; 270–275.
- Nieder, G.L., Parmelee, D.X., Stolfi, A., Hudes, P.D. TBL in a medical gross anatomy and embryology course. Clin Anat 2005; 18: 56–63.
- Dunaway, G.A. Adaption of team learning to an introductory graduate pharmacology course. Teach Learn Med, 2005; 17: 56–62.