ABSTRACT
Students have variable and sometimes multimodal learning preferences that include kinesthetic (i.e. hands-on or tactile) learning. Yet the pre-clerkship medical school curriculum does not emphasize kinesthetic learning of basic science, particularly content in modern genetics, cell biology, immunology, pharmacology and nutrition. A new instructional strategy to enhance kinesthetic learning of basic science is the Basic Science Learning Station. At the Learning Station, students experience weekly self-guided activities which include the physical manipulation of games, puzzles and conceptual models. The Learning Station modules provide opportunities for students to integrate basic science information, reinforce concepts presented in other formats (i.e. lecture or case-based), and provide motivation and enthusiasm for basic science learning. Furthermore, the Learning Station kinesthetic strategy provides a new curricular structure in which basic science faculty can design ways to help students integrate clinical and basic science content domains. Our students report they enjoyed the hands-on approach to learning.
INTRODUCTION
The teaching of the basic science foundation in medical school has historically been divided into discipline-specific departments and courses, such as anatomy, physiology, pharmacology, etc. With the emergence of understanding in cellular and molecular-based disciplines (i.e. genetics, cell biology, immunology, pharmacology and nutrition), the expansive basic science “foundation” of medical care has been progressively squeezed into the same two-year duration of training. In an effort to integrate the traditional “silos” of information, pre-clerkship medical school curricula have also evolved, leading to cross and inter-disciplinary courses such as “Brain, Mind, Behavior”; “Metabolism and Nutrition”; and “Infection, Inflammation, and Immunity.”1
This revised curricular structure may have achieved some degree of success integrating basic science content. But concurrently there has been an expansion of clinical experiences earlier in the pre-clerkship basic science coursework. Consequently, there has been a progressive decline in the time devoted to basic science laboratory or hands-on experiences (e.g. dissection of cadavers, experiments involving laboratory animals, etc.). In some cases, the hands-on laboratory component of the curriculum has been largely replaced by computer simulation or eliminated altogether.2,3 Even those laboratory sessions that still remain often prioritize visual or analytical skills with fewer and fewer hands-on approaches that rely on instructor-led demonstrations, prosections, sample patient-volunteers, or passive observations by the target learners.2,3
It is these twin forces of content explosion and passive-learning methods that have diminished the hands-on basic science curriculum in many medical schools including our own small experimental program called the UC Berkeley – UCSF Joint Medical Program (JMP). The JMP enrolls 12-16 medical students per year who complete pre-clerkship years at UC Berkeley before going on to UCSF for the clerkship years. The JMP curriculum distributes the usual two-year pre-clerkship curriculum across three years because the students simultaneously pursue a master’s degree in health sciences during this time. In 2002, the JMP consolidated the entire pre-clerkship basic and clinical course structure into a comprehensive Problem-Based Learning (PBL) curriculum consisting of a series of paper-based clinical cases.
In order to address the need for hands-on basic science learning, we created a new curricular concept called the Basic Science Learning Station. Medical students attended this ‘Learning Station’ as a parallel activity to supplement the paper cases in the first and second years of our pre-clerkship curriculum. We developed sixteen independent modules to help students integrate and learn basic science information. In this article, we describe the creation and development of the Learning Station, and provide data regarding student evaluations of the Learning Station experience.
NEW APPROACH
Beginning in 2003, we set up the Learning Station in our program during the fall semesters and report here our experiences for the first five years of its existence. The first and second-year classes of medical students (n = 24 – 32 students) were invited to voluntarily participate in the Learning Station. The weekly module at the station was presented as an optional un-graded formative activity, but attendance was encouraged by faculty. Each weekly module was designed to overlap or provide enrichment to the basic science areas related to the corresponding PBL case for that particular week. The modules were presented to first and second-year students on alternate weeks, resulting in an average of 8 learning stations per cohort per academic year. The Learning Station was available to all students for four business days per week between the hours of 8am – 5pm.
The Learning Station was designed to be a ‘dry lab’ physically situated in a 7’x12’ cubicle with surrounding wallboard in an open suite of adjoining offices. Furniture was simple and consisted of a 24” depth L-shaped 36” high table with approximately 12 linear feet of table space and rolling chairs. Permanent equipment included a small refrigerator, microscope, slide viewer and microcomputer.
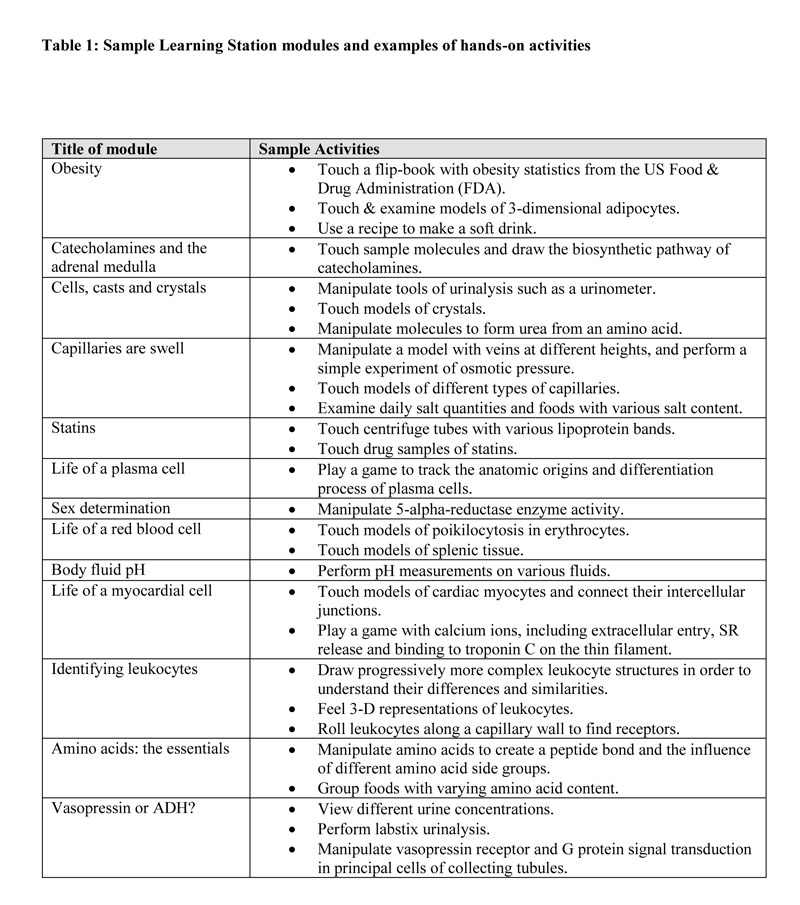
Each weekly module was arranged as a progression of 4-7 activities, consisting of items such as original hand-made models, games, puzzles, foods, containers and objects placed on the table top. An instruction booklet facilitated students through these self-guided, self-paced activities (see Table 1 for descriptions of sample Learning Station activities). The students were invited to touch or manipulate the objects in order to illustrate a scientific concept or facilitate their performance of a simple experiment. In addition, approximately 50% of the station modules contained a histology tutorial component consisting of 10-12 annotated light and electron photomicrographs (on computer, slide carousel or hard copy), as well as one glass slide for hands-on viewing with the microscope. Students could work solo, in pairs or small groups as desired. Each specific module was designed to be completed in approximately 10-20 minutes.
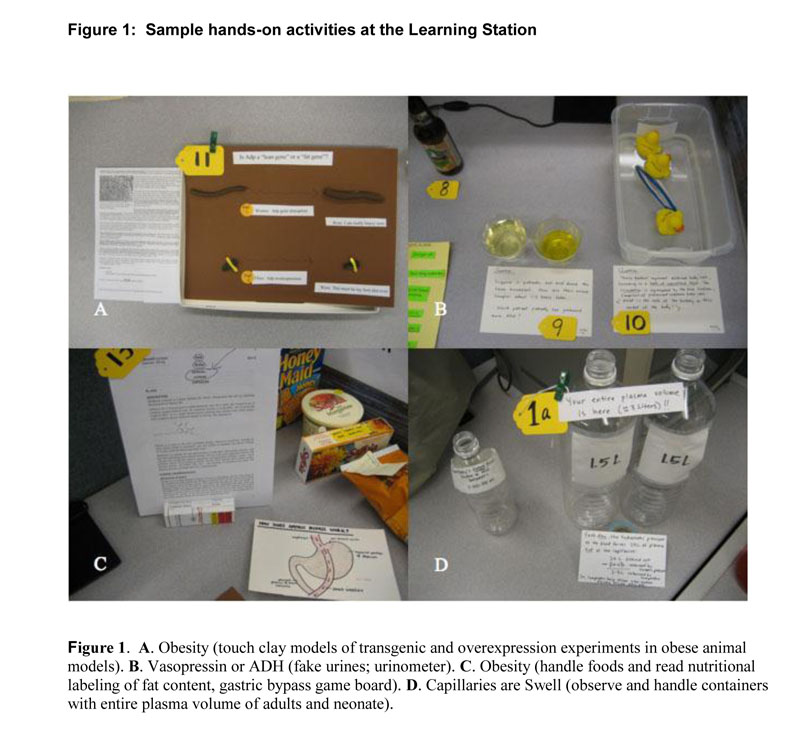
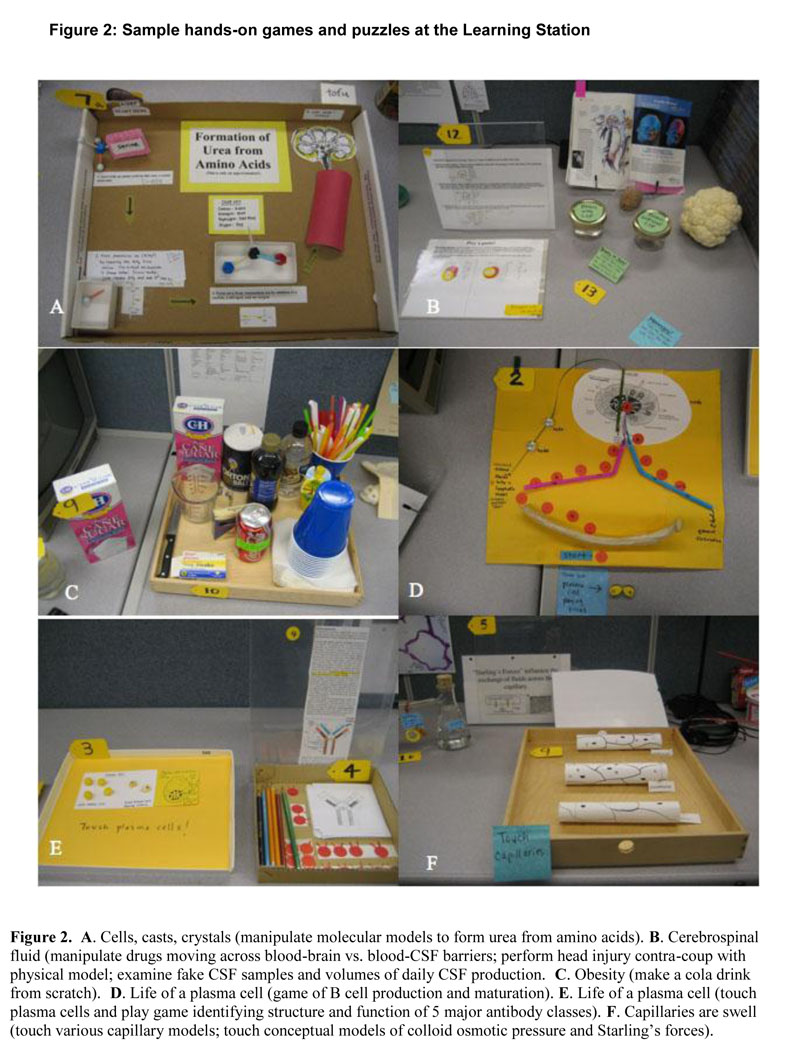
Many of the activities at the station involved the hands-on manipulation of objects or models which were constructed in advance using very simple materials such as paper, plastic, wood, glass containers or everyday objects. These models represented abstract molecular processes, conceptual information, or dynamic cellular activities which students performed by touching or altering the objects (see Figure 1 for examples). Students were also asked to touch hand-made puzzles or play board games comprised of tissue or organ drawings as representations (see Figure 2 for examples). Nutritional items such as vitamin supplements, food labels, pharmaceutical containers and real foods or facsimiles were also displayed.
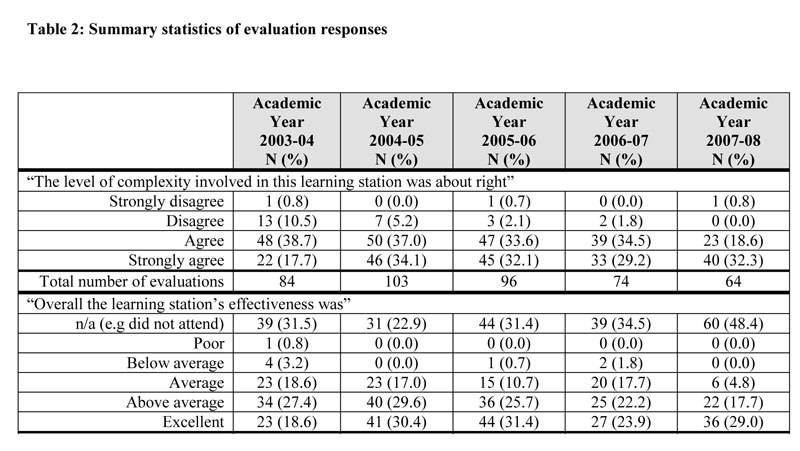
To evaluate the Learning Station, students were required to fill out an electronic questionnaire each week, regardless of their attendance at individual stations. The questionnaire included open-ended questions, as well as items with 5-point Likert scales. One question asked respondents whether the level of complexity of the learning station was appropriate, and response options ranged from “strongly disagree” to “strongly agree.” A separate question asked about the station effectiveness, and response options ranged from “poor” to “excellent.” If students did not participate in individual stations, they were encouraged to answer “not applicable” to the questionnaire items.
PILOT DATA
Even though the station was a completely optional activity, roughly 3 out of 4 students regularly attended the station modules. Since 2003, the percent of students who interacted with the station ranged annually from 57 – 77% attendance. The 2007-08 academic year showed the lowest student participation (i.e. 57% of the students filled out evaluations) although it is not clear to us why this unanticipated drop occurred. The aggregate of student responses to the Likert questions in the evaluation questionnaire across all learning stations is provided as Table 2. Although not robustly designed to be an educational research study, these summary statistics provide some evidence in support of the educational value of the station.
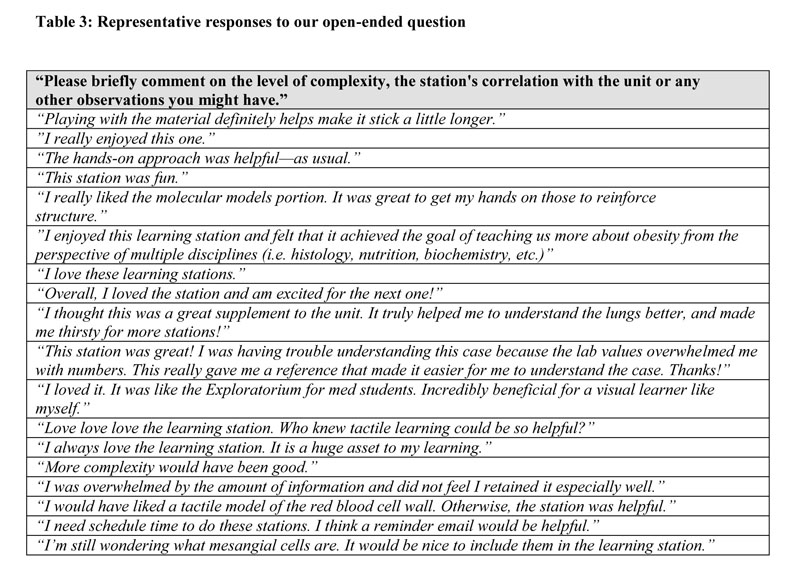
A sampling of student responses to open-ended questions is provided in Table 3. Many students clearly valued the learning station as part of their learning process in this case-based curriculum. In describing their thoughts, the word ‘love’ appeared many times over, indicating how passionately some students felt about this experience. Although far less frequent, students also offered constructive criticisms or neutral comments about the station which could be roughly broken down into three main categories: 1) insufficient time in their schedules to complete the station, 2) desire for a different complexity of material (either more or less), and 3) specific suggestions to improve the station by creating specific new hands-on models or materials.
LIMITATIONS
There are several limitations to our analyses. First, this effort was not robustly designed to be a scholarly evaluation or education research study. We did not, for example, include a matched cohort of students in PBL without the Learning Station opportunity. Our success in establishing the learning station may well have been influenced by our small size (n=16 students average per year), and include a variety of factors inherent in a small class per se. For instance, collective learning is a common thread and the activities that are enjoyed tend to be passed along to the group through amplification. We may also attract certain students that might be either over-or under-represented in certain ways in a larger program where there is more anonymity. Our reputation as an experimental program might skew our enrollment towards those who prefer atypical or novel approaches to learning, especially our extensive PBL curriculum. And since this was a voluntary activity, another limitation is the variable response rate for Learning Station participation and evaluation each year. Some students completed the Learning Station without evaluating the activity, while other students may have completed the evaluation without participating in the Learning Station.4
During the initial year (2003), second-year medical students who had not experienced the Learning Station in their prior academic year had the lowest satisfaction rate. This suggests that initiation of a new approach such as the Learning Station might fare better with first-year students. Additionally, students who enjoyed the station likely contributed to a response bias. In this report we did not present evaluation data of each station individually. Consequently the results in Table 2 suffer from “regressing to the mean,” and therefore may not accurately represent the true variation in student opinions about each individual station.
As our curriculum has no formal laboratory component, the results may be irrelevant to schools with laboratory curricula. Thus, our students, as well as their responses about the Learning Station, are likely a non-representative sample of pre-clerkship medical students. Furthermore, since our evaluations were anonymous, we don’t know the impact of the Learning Station on knowledge retention among individuals. Neither do we have correlative data for individual board performance or clinical skills. In spite of these limitations, we noticed a strong and consistent level of participation and satisfaction by our students over a 5-year period.
SUMMARY AND DISCUSSION
The Learning Station directly addresses medical student desires for kinesthetic learning opportunities through an innovative approach to teaching basic science. In the education literature there has been recent interest in student learning styles.4,5,6,7,8,9 One learning style instrument categorizes learning preferences into visual, auditory, read-write or kinesthetic. Many individuals have multimodal preferences (i.e. two or more preferences).10 According to recent studies using this instrument, approximately 2/3 of first-year medical students have multimodal learning preferences, and most of these students have a kinesthetic preference among their multiple preferences.11,12 The remaining 1/3 of the medical students prefer a single mode of learning, and the largest percentage of those students favor kinesthetic learning. Our data, together with the above evidence from the literature, suggest that a great number of medical students—perhaps the majority—would benefit from or even prefer hands-on activities for learning basic science such as those presented at the Learning Station.
Our approach can be adopted and scaled up to a larger medical school basic science program. If implemented, it would provide: 1) a low-cost creative solution for active kinesthetic learning without the traditional ‘wet lab’, 2) reinforcement of concepts introduced in either lecture, small group, or PBL cases, 3) opportunity for enrichment in basic science areas under-represented in the lab curriculum (e.g. genetics, cell biology, immunology, pharmacology and nutrition), 4) a space-saving compact learning environment available to students at variable open-lab hours without an instructor present, and 5) self-directed learning (SDL) which provides exploration and discovery. The SDL method is an effective science learning tool10 and has been shown to correlate with clinical performance.11
The Learning Station also presents new opportunities for presenting cross-disciplinary basic science content with clinical context. This approach may inspire and motivate students to acquire and retain basic science knowledge longer than they might otherwise.12 This is particularly valuable in light of the recent deliberations by the National Board of Medical Examiners (NBME) to convert the United States Medical Licensing Exam (USMLE) Steps 1 and 2 into a single “Gateway” exam.13 Further work is needed to define in more detail the ways in which students benefit from the Learning Station, and whether it helps students retain basic science conceptual information during their clerkship years and beyond.
There is no doubt that current pre-clerkship basic science curricula broadly continue to rely heavily on the lecture-based didactic format. Learning of basic science through lecture may create a mismatch between student learning and instructor teaching styles, particularly for students who prefer kinesthetic learning. This raises concerns about students who fall short of program expectations4, or have low retention of basic science content.12 Kinesthetic activities, such as those presented at the Learning Station, may even enhance preparation of students for procedure-based clinical specialties such as surgery, obstetrics and emergency medicine.
Development of a new Learning Station by other institutions may require a significant initial time commitment by basic science faculty to acquire or create materials, and later to continually upgrade the modules. Although students and faculty may initially resist a new curricular component with a completely new structure, we are heartened by the evaluation of our learning station by one of our first year students, completed even before his/her participation in any learning station:
“I was very impressed by the amount of thought that goes into the learning station—it looks appealing and accessible.”
Sample learning station modules can also be obtained at the website http://jmp.berkeley.edu with Learning Station author’s permission (JB).
ACKNOWLEDGEMENTS
The authors wish to thank John Swartzberg and Tom Boyce for support of the JMP Basic Science Learning Station, Kevin Mack for encouragement and data acquisition, Tiffany Yuan and Diane Fong for technical support, Nina Green for photography and students in the JMP for participation and feedback.
REFERENCES
- Loeser, H., O’Sullivan, P., and Irby, D.M. Leadership lessons from curricular change at the University of California, San Francisco, School of Medicine. Academic Medicine. 2007; 82(4): 324-330.
- Curriculum Management & Information Tool. Association of American Medical Colleges: http://www.aamc.org/meded/curric/start.htm. [Accessed 11/06/2008]
- Salas, A.A., Anderson, M.B., LaCourse, L., Allen, R., Candler, C.S., Cameron, T., and Lafferty, D. CurrMIT: a tool for managing medical school curricula. Academic Medicine. 2003; 78(3): 275-279.
- Curry, L. Cognitive and learning styles in medical education. Academic Medicine. 1999; 74(4): 409-413.
- Coffield, F., Moseley, D., Hall, E., and Ecclestone, K. Should we be using learning styles? What research has to say to practice. www.LSRC.ac.uk [Accessed 09/04/2008]
- Hendricson, W.D., Berlocher, W.C., and Herbert, R.J. A four-year longitudinal study of dental student learning styles. Journal of Dental Education. 1987; 51(4): 175-181.
- Du, Y., and Simpson, C. Effects of Learning Styles and Class Participation on Students’ Enjoyment Level in Distributed Learning Environments. Journal of Education for Library and Information Science. 2004; 45(2): 123-136.
- Sandmire, D.A., and Boyce, P.F. Pairing of opposite learning styles among allied health students: effects on collaborative performance. Journal of Allied Health. 2004; 33(2): 156-163.
- Wehrwein, E.A., Lujan, H.L., and DiCarlo, S.E. Gender differences in learning style preferences among undergraduate physiology students. Advances in Physiology Education. 2007; 31(2): 153-157.
- Abraham, R.R., Upadhya, S., and Ramnarayan, K. Self-directed learning. Advances in Physiology Education. 2005; 29(2): 135-136.
- Shokar, G.S., Shokar, N.K., Romero, C.M., and Bulik, R.J. Self-directed learning: looking at outcomes with medical students. Family Medicine. 2002; 34(3): 197-200.
- Ling, Y., Swanson, D.B., Holtzman, K., and Bucak, S.D. Retention of basic science information by senior medical students. Academic Medicine. 2008; 83(10 Suppl): S82-S85.
- Fuchs, E. Changes Possible for Medical Licensing Exam. Association of American Medical Colleges: http://www.aamc.org/newsroom/reporter/dec07/usmle.htm [Accessed 12/11/2008]