ABSTRACT
The field of medicine requires a lifelong commitment to education, both as a student and as a teacher. The role of medical students in teaching as well as course design has seldom been explored. As part of a curriculum change at our institution, senior medical students were integrally involved in designing, implementing, and teaching a new first year pathology course focused on independent learning. Before the 2006-2007 and 2007-2008 pathology course, the course director chose four to five senior medical students to act as teaching assistants (TAs). TAs met with the course director multiple times to discuss new course components. Due directly to involvement of the TAs, the 2007-2008 pathology course consisted of five components: lectures, small group sessions, journal club sessions, podcasts, and student case presentations. After the 2007-2008 pathology course, 41 of 42 students completed a subjective survey assessing the course as well as the use of senior medical students as TAs.
This study documents senior students operating effectively as both teachers and course designers. It also serves as a blueprint for student course designers to implement and evaluate changes and foster a culture of peer teaching. It demonstrates that first year medical students are comfortable with senior medical students as teachers; furthermore, these students have an increased interest in teaching as a result of the course. This involvement of senior medical students in the teaching and course design process may foster a culture of peer teaching and leadership that would benefit medical students, their peers, and potentially their patients.
INTRODUCTION
Medical education is a constantly evolving discipline. This has been illustrated in the last three decades, during which trends in education methods have moved away from lengthy lectures toward problem-based learning (PBL) and more recently, team-based learning (TBL)1-3. In the case of PBL and TBL, studies have demonstrated improved student attention, comprehension, and enjoyment4,5. These positive results have led to the widespread adoption of these methods in medical school curricula across the country. Broad changes in teaching ideology are generally implemented from the top down; however, at every institution these tools must be refined to fit specific student and classroom needs. Quality improvement (QI) initiatives and 360 degree evaluations attempt to evaluate individual courses in order to improve teaching methodology on a classroom level, but changes are often either too small or too slowly implemented to be of benefit.
Although the Accreditation Council for Graduate Medical Education (ACGME) recognizes the critical role of residents as educators for both graduate and undergraduate medical education, there have been relatively few studies that describe how undergraduate medical students develop skills that are critical for their development as educators6. At almost all medical schools, students play a significant role in the evaluation of courses and clerkships. However, their role is often a passive one, restricted to filling out critiques addressing faculty identified strengths and weaknesses of the curriculum. In spite of this, medical students who have recently completed the course are often in the best position to identify the most efficient methods to facilitate learning of the material. Direct involvement of students gives the potential to swiftly design and implement changes specifically desired by students. Engaging in the process of curriculum reform requires students to reflect on current limitations and potential areas of improvement, formulate a plan, and act on that plan. Thus in addition to improving existing courses, this process cultivates leadership skills.
Our institution recently restructured and revamped the first two years of the medical school curriculum, implementing student-directed and team-based learning ideas from PBL and TBL formats. The curricular changes also aim to better prepare students for the challenges of 21st century medicine. Inherent in these changes is the vision that medical students will become effective leaders and team members who improve processes, improve outcomes, and think creatively to advance medicine through innovation and education. With this in mind, we provided senior medical students with the opportunity to develop and implement several novel learning techniques in a cell biology and pathology course taught to first year medical students.
Nine senior medical students restructured the first year cell biology and pathology course. The result was a hybrid format of high-yield lectures and small-group learning sessions. In addition, several initiatives were developed by third year students to provide first year students with additional learning tools. Development of learning tools took into consideration many different learning styles7, which were divided into three broad categories: auditory, visual, and kinesthetic. To appeal to these major learning styles we included a twice weekly podcast review, a biweekly clinical journal club, and student case presentations. These teaching tools have been widely used and studied in the past. Podcasts have been used by medical journals to report weekly news to medical personnel, by major medical centers to educate a general audience, and by educational centers for continuing medical education8-10. More recently, the use of podcasts in the classroom has been studied, and well received by medical students without any decrease in class attendance11. Similarly, journal clubs have been widely used in residencies to teach skills in clinical data interpretation12.
Here we report the renovation and evaluation of an introductory pathology course at Mayo Medical School executed primarily by medical students, with teaching responsibilities shared between senior medical students and faculty.
METHODS
Selection of Teaching Assistants
Before the 2006-2007 and 2007-2008 academic years, the course director for the first year Pathology and Cell Biology course selected four or five interested medical students in the clinical years (years 3 and 4) to act as teaching assistants. Teaching assistants (TAs) planned their clinical schedules such that teaching time overlapped with research time, protected from clinical responsibilities. A twelve week research block is included in our institution’s third year schedule.
TAs formed a committee before the course began to develop methods to reduce contact hours, increase learner autonomy, and provide students with appropriate tools to allow them to efficiently and effectively learn pathology. TAs then met with the course director to discuss implementation of new ideas, and together developed the course schedule for the academic year.
Pathology and Cell Biology 2006-2008
From 2006-2008, the Pathology and Cell Biology course at Mayo Clinic College of Medicine was trimmed from a twelve week to a six week long course. The course covers cellular homeostasis and reactions to stimuli that disrupt homeostasis and lead to disease. Specific topics include homeostasis, intracellular accumulation, necrosis, inflammation, hemostasis and hemodynamics, and neoplasia. Approximately forty-two students enroll in the course each year. Six to eight hours per week of lectures are conducted by the course director, decreased significantly from ten hours per week in previous years.
Small group laboratory sessions
Previous iterations of the Pathology and Cell Biology course included weekly laboratory sessions, which allowed students to work independently through microscopic slides and question sets in order to apply principles learned in class to both gross and microscopic specimens.
For the 2006-2007 and 2007-2008 academic years, these independent laboratory sessions were replaced by twice weekly small group sessions designed by medical student teaching assistants. Students were divided into groups of ten to eleven, with each group led by a senior medical student-teacher. These sessions consisted of a brief overview presentation followed by three to four clinical cases with correlating microscopic and gross specimens. Sessions covered gross and microscopic changes as well as laboratory and clinical findings. Each case incorporated a clinical history, gross specimens, virtual microscopy (presented on classroom smartboards and individual laptops), and questions for discussion. Topics, cases, images, PowerPoint slides, and questions for each small group session were selected by the course director and were common to all small groups. Student-teachers met 2 to 5 days before sessions to discuss the questions, important concepts, and clinical correlations to ensure homogeneity of small group sessions. The course director was available when questions among TAs arose. Prior to each session students were provided with the clinical history and discussion questions. Students were encouraged to review the case in order to allow for efficient learning. Students worked in groups facilitated by the student-teacher, who was responsible for ensuring that major teaching points were covered. Student-teachers were used not to answer the questions, but to facilitate discussion where the students shared their own answers. A total of ten small group sessions were held.
Podcast review session
For the 2007-2008 academic year, the TAs developed new, concise (15 to 25 minute) review sessions covering key concepts and example cases. Reviews were recorded as digital audio (podcasts) and distributed in coordination with topics covered in lectures and small group sessions. Podcasts were released twice weekly and were available to students throughout the course. Podcasts were recorded using a free-for-download program (Audacity™) in Wave Audio Format (.wav), and were encoded in MPEG-1, Audio Layer 3 (.mp3) at 128kbps. They were then distributed internally using both the course website and the Mayo Clinic intranet.
Clinical problem solving sessions
In the 2007-2008 academic year, a clinical problem-solving journal club was developed by the TAs and held three times throughout the course. Students were divided into groups of ten and were asked to work through cases from the New England Journal of Medicine “Clinical Problem-Solving” section13-15. Sessions were led by TAs who encouraged students to interpret clinical data with a focus on clinical decision-making. The major emphasis of these sessions included formulating a differential diagnosis and choosing diagnostic tests. At the conclusion of each case, there was a five-minute discussion of relevant pathologic findings.
Student case presentation
Students were divided into groups of 3-4 and given a pathologic case to solve, including a brief history of present illness and several pathology slides. Each group prepared a presentation on their assigned clinical case and delivered this presentation to their classmates. Case presentation sessions were conducted by the course director. These case presentations were unchanged from previous years.
Evaluation of teaching modalities
Upon completion of the 2007-2008 course, all students were invited to complete a brief, anonymous questionnaire regarding their perceptions of the course. This non-validated questionnaire was designed by the student-teachers as a device to evaluate their contributions to the course. The questionnaire asked students to rank their level of agreement with various statements on semantic differential scales from 1 to 10, with 10 being complete agreement. Students were questioned in this manner on their preferred learning style (Visual, Auditory, and Kinesthetic), as well as on the use of lectures, small group sessions, podcasts, clinical problem solving sessions, and student case presentations. Students were also asked to rank the five course components from in order of usefulness. While the study was not recruited to a power to show a specific level of correlation, correlation calculations between data points was performed using the Fisher’s Exact Test. A cut-off value of 7 or greater on scales of 0 to 10 was used to distinguish between responses that were “strongly in agreement” and those that were not for Fischer’s Exact Test. A p value of 0.05 was considered statistically significant.
RESULTS
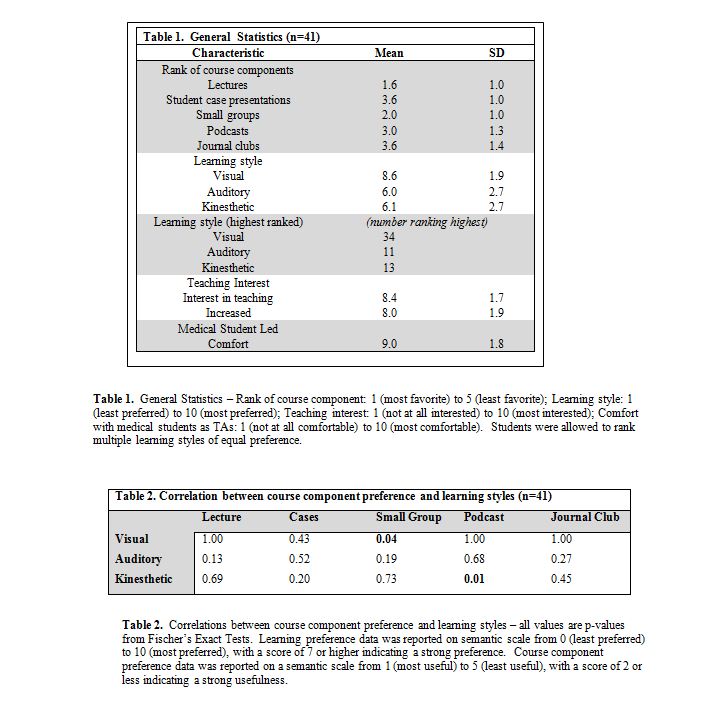
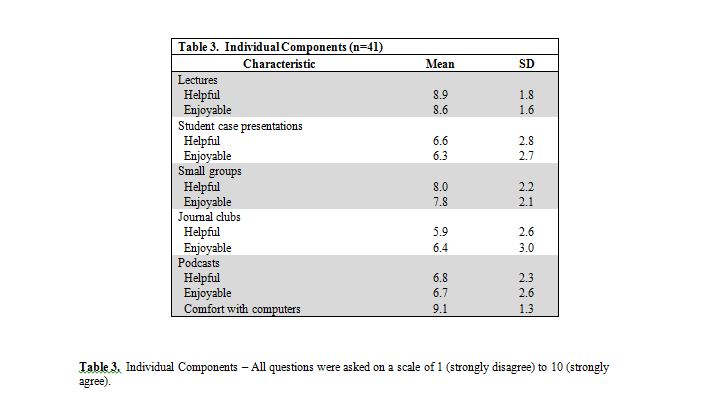
General summary data for our pathology course is outlined in Table 1. Forty-one (41) of 42 students completed the survey. Lectures were viewed as the most important component of the course, followed by the three student led initiatives, with student case presentations ranking as least important. Seventy-three percent (73%) of students preferred lectures less than two hours in length. Most students rated a visual learning style as their preferred format, although a non-trivial minority selected both auditory and kinesthetic.
Students as teachers
The small groups, podcast reviews, and journal clubs were all led by third year TAs. Students were very comfortable with student-teachers conducting these sessions (mean score 9.0/10). At the end of the course, students reported a very strong interest in teaching (8.4/10). Additionally, students reported a greatly increased interest in teaching as a result of the student-led pathology course (mean 8.0/10) (Table 1). Those who ranked TA led small groups highly were also significantly more likely to have increased interest in teaching at the end of the course (p=0.01).
Small groups
Senior medical student-led small groups ranked as the second most important component of the course. Sixty-eight percent (68%) of students attended all of the small group sessions, while 85% of students attended at least seven of the ten sessions. Eighty-three percent (83%) of students preferred small group sessions shorter than three hours. Visual learners found these small group sessions more helpful than non-visual learners (p=0.04) (Table 2). Auditory learners also tended to find these sessions helpful, although this did not reach statistical significance (p=0.19).
Podcasts
Students were generally very comfortable with computers (mean 9.1 / 10, Table 3). A large majority of students (85%) own an iPod or comparable music player, and a majority of students (63%) made use of the podcast reviews. Students preferred a brief length, with 64% preferring less than 25 minutes per podcast and 93% preferring less than 45 minutes. Kinesthetic learners tended to find these reviews more helpful than non-kinesthetic learners (p=0.01).
Journal club
Sixty-one percent of students attended all journal club sessions. Journal club was generally thought to be less valuable than the podcasts, with 44% rating it as the “least valuable” component of the course. A sizeable minority (24%) of students, however, reported it as one of the two most valuable aspects of the course. No correlation was found between learning style and usefulness of journal club. However, students who found it a very helpful part of class reported large improvements in differential diagnosis formulation (p less than 0.01), a greater desire to read medical journals (p less than 0.01), and more excitement for upcoming clinical experiences (p less than 0.01).
DISCUSSION
The methods we use to teach medical science are evolving1. The changes that drive this evolution are typically implemented from the top down, whether from new studies from educational experts, an institution-wide policy change, or a professor changing the way he or she chooses to teach. Our study sought to both implement and evaluate changes from the bottom up, utilizing senior medical students as the key drivers to this end. To our knowledge, the use of senior students as teachers has been little explored6, while their use in curricular changes has not been reported. We found both the changes themselves and the utilization of students as teachers and curriculum designers independently interesting.
New course additions: a student led initiative
The 2007-2008 Pathology course at our institution was successful in allowing student-teachers to create, implement, and evaluate educational innovations. By combining mentorship with autonomy for innovation, the course director was able to harness ideas and energy from senior medical students to implement changes more quickly than might have been possible otherwise. This also encouraged the student-teachers to evaluate their changes to assess what impact, if any, they had on their students.
Before discussing the results of our survey outlined above, we must note this survey was performed for use by the student-teachers to evaluate their changes and has not been validated elsewhere. We also used student preferences as our endpoint, as opposed to a hard endpoint such as test score. Similarly, our study population was defined by our class size (42), and hence was not powered to show specific levels of correlation; significant correlations were potentially missed. We must also note that these findings are potentially relevant only to our own medical school.
These facts not withstanding, there are a few conclusions that can be drawn. While many medical school curricula – including our own – are moving away from the all-day lecture format, lecture still rated as the most important aspect of our course. We attribute this to the ever expanding extent of medical knowledge leading to a need for direction towards important concepts and away from triviality. However, the length of time spent in lectures should be kept concise. In fact, ‘short and sweet’ seems to be an excellent motto for all components to the course, including lectures, small groups, journal club, and podcasts.
It is well established, and in fact common sense, that different learners prefer different learning styles7 and different learning tools. In an independent learning curriculum where students are asked to self-teach, it is important to make a wide range of tools available. These should contain traditional tools, such as lectures and textbooks, but should also encompass alternatives. Today’s students are exceedingly comfortable with technology; perhaps even more so than their instructors. Thus technologically advanced tools such as virtual histology and podcasts should be available. Similarly, with the pace of advancements in medical sciences, it is important to begin reading primary literature early in medical education. We demonstrated a course design with these multiple elements geared towards different styles of learners. Virtual histology-based small group sessions were significantly favored by visual learners, while brief podcast reviews were favored by kinesthetic learners. Correlations between auditory learners and preference for lectures and between kinesthetic learners and case presentations were present, although they did not reach statistical significance. This is potentially due to a lack of power in this study. Further work, potentially using test scores instead of student preference as the endpoint, are needed to elucidate these potential correlations.
These multiple learning tools do come with an important caveat. With the proliferation of educational materials and the increased role of self-directed learning, there is the potential for students to try to do too much. It is important for students to choose the tools that work best for them to learn the material, and not try to use everything available. Despite this potential pitfall, however, multiple learning tools in the classroom appear to be of benefit in a self-directed curriculum.
Medical students as teachers and course designers
A key aspect of our course changes was that medical students became teachers and drivers of course improvements.
Physicians occupy the dual role of learner and teacher throughout their careers. The field of medicine requires physicians to be lifelong learners, and physicians are in turn responsible for teaching patients, families, and colleagues. It seems appropriate to begin cultivating teaching skills early in a physician’s career, beginning in medical school.
Our study demonstrates that first year medical students were comfortable learning from peers in the introductory pathology course, and that as a result of this course students had an increased interest in teaching. We believe that first year students, senior students, and future patients of these students may all potentially benefit from this type of course structure in which students are given the opportunity to develop teaching skills and take responsibility for improving the existing structure through curriculum reform.
First year students gain early insight into opportunities for teaching in medicine and may develop personal interest in teaching. They also gain early exposure to peer teachers and students who are taking action to improve courses. This helps to create a culture of continuous quality improvement and peer-teaching. As first year students advance through their medical education, it will become their responsibility to add or improve upon course components for future students.
Senior students gain invaluable experience as teachers. In addition to developing teaching skills, students also gain experience in leadership and innovation through taking responsibility for conscious re-evaluation and improvement of existing courses. Even patients may benefit from a cadre of physicians who have had an early opportunity to develop teaching skills and consciously evaluate and improve existing structures.
The changes that medical students were able to effect in this introductory pathology course would not be possible without an institutional culture conducive to student-teachers and student-driven reform. Our medical school has a long history of utilizing medical students as teaching assistants16. By involving students who recently completed the same courses, our teaching staff gains perspective on which aspects of their courses were effective and useful for students and which need modification. Student-driven curricular reform, as exemplified in this introductory pathology course, allows a curriculum to quickly adapt to changing needs and preferences of students, provides valuable teaching experience to student-teachers, and encourages conscious and continuous curricular improvement that benefits future students.
Further scientific analysis is needed to assess the utility of both this multifaceted approach to teaching pathology, as well as the utility of senior student led small groups and student-led initiatives. However, our data indicate that students appreciate a variety of different learning tools and that student-teachers and student-led initiatives cultivate teaching interest in first year medical students. This approach to medical education may foster a culture of peer teaching and leadership that would benefit medical students, their peers, and potentially their patients.
REFERENCES
- 1.Donner, R.S., and Bickley, H. Problem-based learning in American medical education: an overview. Bulletin of the Medical Library Association. 1993;81(3):294-298.
2.Su, A.Y. The impact of individual ability, favorable team member scores, and student perception of course importance on student preference of team-based learning and grading methods. Adolescence. 2007;42(168):805-826.
3.Thompson, B.M., Schneider, V.F., Haidet, P., Levine, R.E., McMahon, K.K., Perkowski, L.C., and Richards, B.F. Team-based learning at ten medical schools: two years later. Medical Education. 2007;41(3):250-257.
4.Albanese, M.A., and Mitchell, S. Problem-based learning: a review of literature on its outcomes and implementation issues. Academic Medicine. 1993;68(1):52-81.
5.Vernon, D.T., and Blake, R.L. Does problem-based learning work? A meta-analysis of evaluative research. Academic Medicine. 1993;68(7):550-563.
6.Streips, U.N., and Atlas, R. Fourth year students are effective case discussion leaders. Journal of the International Association of Medical Science Educators. 2001;10:23-26.
7.Coffield, F., Moseley, D., Hall, E., and Ecclestone, K. Learning styles and pedagogy in post-16 learning. London: The Learning and Skills Research Centre; 2004.
8.Abbasi, K. Journals join the podcast revolution. Journal of the Royal Society of Medicine. 2006;99(7):329.
9.Abreu, D.V., Tamura, T.K., Sipp, J.A., Keamy, D.G., Jr., and Eavey, R.D. Podcasting: contemporary patient education. Ear Nose Throat Journal. 2008;87(4):208, 210-201.
10.Ragon, B., and Looney, R.P. Podcasting at the University of Virginia Claude Moore Health Sciences Library. Medical Reference Service Q. 2007;26(1):17-26.
11.Pilarski, P.P., Johnstone, A. D., Pettepher, C.C., and Osheroff, N. From music to macromolecules: using rich media/podcast lecture recordings to enhance the preclinical educational experience. Medical Teacher. 2008;30(6):630-632.
12.Rinder, H.M., and Smith, B.R. Innovative methods in laboratory medicine resident teaching. Clinical Laboratory Medicine. 2007;27(2):255-267; abstract vi.
13.Clarke, P., Glick, S., and Reilly, B.M. Clinical problem-solving. On the threshold–a diagnosis of exclusion. New England Journal of Medicine. 2005;352(9):919-924.
14.Thomas, L.R., Baden, L., and Zaleznik, D.F. Clinical problem-solving. Chest pain with a surprising course. New England Journal of Medicine. 1999;341(15):1134-1138.
15.Rozenman, Y., Gilon, D., and Fuchs, S. Clinical problem-solving. Where did good old clinical diagnosis go? New England Journal of Medicine. 1997;336(20):1435-1438.
16.Ocel, J.J., Palmer, B.A., Wittich, C.M., Carmichael, S.W., and Pawlina, W. Outcomes of the gross and developmental anatomy teaching assistant experience. Clinical Anatomy. 2003;16(6):526-530.