ABSTRACT
Increasingly, medical educators are turning their attention and efforts toward enhancing the professionalism of medical students, starting with their first year of medical school [1]. Key to this endeavor is the development of educational structures and opportunities for ongoing reflection on practice. Scholars of how professionals in all fields think in practice, emphasize the continual cycles of reflection and action in which professionals engage as they hone their practice and improve the effectiveness with which they work with clients. Donald Shön, a leading figure in this field, speaks of reflection-on-action and reflection-in-action as hallmarks of professional habits of mind [2]. This article argues that structured research activities, woven into the medical school curriculum from the first year on, can foster the habits of mind associated with professionalism. Reflective practice can be seen to exist on a continuum with the more focused and rigorous systematic inquiry distinctive of research. Furthermore, this reflective practice is progressively entrenched and strengthened as students assume increasingly complex and autonomous roles in communities of inquiry, learning, and research [3, 4]. We present the research program at Case Western Reserve University School of Medicine (CWRU SOM) University Program as a model for how such student research activity situated in authentic research communities can be made an integral component of the medical school curriculum. The medical student research component of the curriculum has only this year been fully implemented, but we have already observed that the structured research activities of this curriculum, in conjunction with other aspects of the curriculum (including the use of a problem-based learning approach and a portfolio process), are effective in cultivating reflective habits of mind and engaging students in authentic ways in communities of inquiry and research, thereby strengthening medical student professionalism.
INTRODUCTION
REFLECTIVE PRACTICE AND THE PRACTICE OF RESEARCH IN MEDICINE
A hallmark of professionalism, as described by Donald Shön [2] in The Reflective Practitioner, is a habit of reflectiveness yoked to strategic action in one’s field. As Shön puts it:
The practitioner allows himself to experience surprise, puzzlement, or confusion in a situation which he finds uncertain or unique. He reflects on the phenomenon before him, and on the prior understandings which have been implicit in his behavior. He carries out an experiment which serves to generate both a new understanding of the phenomenon and a change in the situation. (Schön 1983: 68)
For the medical professional, the change in the situation desired is a positive change in the health status of the patient. Instead of calling it an “experiment,” it would be more consistent with the ethics and mores of the medical profession to call the action a strategic action informed by best thinking in the field of medicine. Nonetheless, it has the same function as Shön’s experiment: it both helps the professional taking the action improve his or her understanding of the phenomenon and changes the situation itself.
This is the key point: the medical professional integrates strategic action with an attitude of reflectiveness aimed at understanding, promoting, and evaluating a change in a patient’s health status. In fact, if the action taken by the medical professional is to be truly strategic, it must, by definition of strategy, be informed by a systematic effort to understand the reasons for the changes in the patient’s health status as a consequence of the action. Coming to this understanding of change requires the medical professional to engage in thinking about at least three essential aspects of the change: 1) to become clear about what is changeable in a patient’s situation – that is, the parameters of health, well-being, and disease that have been or can be modified; 2) to explore the mechanisms and processes by which change occurs and the actions that can be taken to modify factors influencing the patient’s situation; and 3) to be alert to the health outcomes and conditions that emerge as the change process unfolds. This is the fundamental thought process carried out in developing, implementing, and continually adjusting the diagnosis, treatment, and prognosis for a patient, but is construed more generally as a process of constructing an understanding of change in a patient’s health status, which is at the heart of the strategic action informing, and emerging from, reflective habits of mind.
The medical professional’s commitment to a focused and sustained effort targeted at understanding changes in the health status of a patient requires ongoing and systematic inquiry. This effort enmeshes the medical professional in repeated and often overlapping cycles of reflection and action that characterize professional thinking; a continual interplay is set up between reflection-in-action and reflection-on-action. Such systematic inquiry can exist in a continuum with more formal research activity: as questions or puzzlements arise in practice, these can be taken as fodder for focused research. They can be formulated clearly and explicitly – in measurable terms – as questions that drive research. It is, then, a natural next step for the medical professional to think of ways to gather data that will address his or her question as this inquiry unfolds. The professional analyzes the data, looking for clues to the nature of the change that he or she observes in the patient health status; the range of what can change and ways to characterize those changes; the factors that appear to bring about the changes; the measurable effects of action taken; and the conditions and results that emerge as the patient’s health evolves. Thus, there has been an organic movement from more general reflection on clinical practice to more systematic studies of practice, which can take the form at one end of the continuum as formal research activity. All the action-oriented, inquiry-based activities on this continuum mutually reinforce and enrich each other in the context of reflective practice; put another way, action and reflection are seen as integral aspects of a more general reflective practice.
This view of research as existing on a continuum with reflective practice contrasts with an oft-heard belief that appears to set up an opposition between research and practice as separate enterprises. This misguided belief in the opposition of research and practice pervades the larger society as a bias against theoretical knowledge, caricaturing it as a diversion from “real-world” action. Shön’s work is a withering critique of this attitude, identifying as it does the defining characteristic of a profession as the thoroughgoing and continuous integration of reflection and action. Under this view, if members of the medical profession – and aspirants to it, medical students – are to attain professionalism in their work, they must experience the synergy of participation in the creation of emerging knowledge from research and the never-ending honing of one’s clinical practice in the course of their medical careers. This may require a shift in their beliefs about the relationship between research and practice: they may need to move from believing that, in becoming doctors, they first amass a body of theoretical knowledge, demonstrate that they have mastered it in medical school, and then later apply this static, inert body of knowledge in the “real world” of their clinical practice (a belief which feeds back into the notion that research-based knowledge and effective clinical practice are discrete stages of professional growth and development) – to a belief that they are and should be active participants in the creation of knowledge in their field throughout their careers as they continually reflect on and improve their practice. It is this hope and philosophy that animates the medical student research program at Case Western Reserve University School of Medicine (CWRU SOM) University Program.
Goals and Objectives of the Research Program in our Medical School Curriculum
It is in medical school that an orientation to reflection, systematic inquiry, and focused research can be fostered in students. It is the aim of the research component of the CWRU School of Medicine curriculum to cultivate such habits of mind, which will distinguish our graduates as medical professionals.
A number of behaviors make manifest this disposition toward structured reflectiveness. They arise from habits of mind that reveal a commitment to ongoing cycles of reflection and action; a critical but open stance toward emerging knowledge and research; a push to make inquiry increasingly systematic; a propensity to pose interesting questions that emerge from practice (so that issues encountered in patient care provide fodder for research); continually honing or even rethinking practice in light of new perspectives; relentlessly seeking root causes or underlying mechanisms for changes in patients’ health status; and participating actively in the creation of new knowledge.
The desired goals for the medical student research program, aimed at promoting these habits of mind, include the following:
1. Valuing question asking
This is an attitudinal goal that affirms the importance of cultivating the reflective habits of mind associated with medical professionalism. The dimensions of this attitude include an understanding of the reflective habits of mind (a cognitive dimension); an appreciation of the value of these habits (an ethical dimension); and an orientation of one’s behavior to these habits of mind (a dispositional dimension). The reflective habits of mind are worked into a framework of values that informs one’s worldview.
2. Posing good questions
This goal is achieved when students can frame good questions for research, and appreciate the criteria for good questions. They work to make their questions clear and explicit; possess clinical and scientific relevance; lead to testable formulations of hypotheses; and offer new insight in a field. Students need to conduct an adequate literature review to stimulate good questions and to determine if the questions they generate are in fact worth pursuing. Students also keep their ears and minds open for good questions that may emerge in dialogue with peers and faculty members, in interacting with experts in the field, or in pondering puzzles or surprises in clinical encounters with patients.
3. Investigating questions systematically
Achieving the outcome of systematic investigation of questions will be reflected in student ability to formulate plans for their investigation. If they have framed good questions, then the proposal should reflect the formulation of clear, explicit, and testable hypotheses. The proposal should also reflect a working understanding of the range of research concepts, methods, techniques, instruments, and materials common in medical and biomedical research, and critical thinking about the methodologies that could best address the students’ particular questions. At the end of our continuum of reflective practice, working on this goal means being able to investigate one’s questions by conducting hypothesis-driven research, which becomes a key criterion in our assessment of fulfilling the requirements of the research component of the curriculum.
4. Constructing responses to questions with others in a community of inquiry
As students launch in earnest into an investigation of a question, they should continue to think critically about the strengths and limitations of the methodologies that they are employing (working in collaboration with their mentor/principal investigator and his or her team) and the inevitable trade-offs as one designs a research project. On an ongoing basis, students should reflect on and improve their research process, making refinements to (or even rethinking) hypotheses as needed, revisiting protocols, pondering emerging (and perhaps surprising) results, identifying challenges or issues that arise, and engaging in ongoing problem-solving and reflection.
5. Communicating insights into questions to others in a broader community
In addition to contributing constructively to the community of learning, inquiry, and research of which one is a member as a researcher/investigator in a team, our students are also given opportunities to make contributions to the larger field or discipline which the research attempts to advance. Our students build skills in structuring their thinking in research as they learn to write proposals (both for their elective summer research experience and for their mandatory 4-month research block), compose structured abstracts for conferences, deliver presentations, and otherwise communicate their research in conference posters, research reports, grant applications, various articles, and other vehicles.
Key Components of Our Research Program
We help students work toward these goals by providing the following in the CWRU SOM curriculum: 1) the Foundations of Medicine and Health curriculum fulfills a number of research-related learning objectives, which assists students in preparing for their 4-month research block experience; 2) opportunities to conduct summer research after the medical school first year; 3) a four-month research block, where our students commit full-time to work with a mentor identifying research questions, framing methods, carrying out the research, conducting an analysis, and communicating their results in a write-up; 4) often (but not necessarily) building on their work in the four-month research block, students generate a medical thesis, writing up the results of their research in the format of a peer-reviewed journal in their field; and 5) students may take advantage of further opportunities to delve into research, including pursuing dual-degree programs and year-off fellowships. These five areas of the student four-year medical school experience are aimed at fostering professional habits of mind and inuring reflective practice. They represent a coherent developmental trajectory aimed at helping students achieve the above goals and provide a steady increase in challenge in terms of research knowledge and skills, independence in inquiry, and complexity of questions addressed, culminating with the medical thesis.
1. The Foundations of Medicine and Health curriculum
The Foundations of Medicine and Health curriculum, the foundational curriculum in basic and clinical sciences taken in the first year and a half of medical school, covers key concepts in biostatistics and epidemiology; evidence-based medicine; medical informatics; research methods and designs; population-based medicine; and ethical conduct in research, especially issues around informed consent. This curriculum focuses on giving students exposure to the design of clinical trials, the critical appraisal of research findings, the generation of hypotheses in research, the statistical analysis of data and interpretation of statistical measures, the conduct of systematic literature reviews, and an overview of the IRB process and approval.
A Research and Scholarship strand parallels all of the blocks of the Foundational curriculum. In each curricular block (e.g., Block 2 – The Human Blueprint, Block 4 – Homeostasis), researchers from across the campus are invited to speak to students on a bi-weekly basis about a research topic related to the theme of the block. These presentations represent a chance for students to learn more about the range of research opportunities available on campus, the key investigators and centers involved in the research area, and the research problems, methods, and techniques of importance to biomedical research. More subtly, these researchers often expose students to models of physician-scientists who have successfully contributed to research knowledge while remaining active in clinical practice. It is not uncommon for students who later conduct research in a particular field to have first heard about the research opportunity by attending one of these presentations
2. Summer research experience
CWRU School of Medicine incorporates active and meaningful participation in research as an integral part of its medical students’ learning experience. At all steps in their medical school career, medical students are encouraged – and, in the case of the 4-month research block, required – to carry out research under the close mentorship of an experienced researcher in a field that is of interest to them. After their first year of medical school, medical students have a range of opportunities to engage in summer research during an 8- to 10-week period. The Office of Medical Student Research (OMSR) in the CWRU SOM has a full-time director that helps students identify summer research funding opportunities, including three NIH training grants and a private CWRU research fellowship (called the Crile Summer Research Fellowship, available through the Crile Research Endowment at the school of medicine).
With the training grants and the Crile fellowship that OMSR administers, it is required that students take an active part in framing the research questions that they wish to pursue, formulating the methods that they plan to implement in order to investigate those questions, and defining the specific roles and responsibilities that they intend to fulfill in carrying out their research. Students must work with their prospective mentor to craft a proposal that they submit for review by the office. The students should negotiate with their prospective mentors the particular focus, questions, or hypotheses that will structure their study; of course, the work of the student fits in with the larger research agenda of the lab or clinic where they will work, but they define a niche for themselves within that larger context of inquiry. The proposal lays out: 1) an introduction stating what has been established in the field, open questions that remain, and the clinical relevance of the problem or question; 2) a clear statement of the research questions/hypotheses to be investigated; and 3) a section on the methods used for the investigation, including a full statement of the specific roles and responsibilities that students will carry out in the lab or clinic as they do their study.
In our review of their proposals, we place a heavy emphasis on ensuring that students have ownership in the research questions that they pursue based on an intellectual partnership with their mentors; that they develop intellectually substantive skills and knowledge in the conduct of research; and that they have meaningful roles in the research process. We want this proposal writing process to be a learning experience, so we offer coaching before they formally submit their proposals. Students involved in summer research are required to submit structured abstracts of their research at its conclusion. The summer research experiences help to build research knowledge and skills that will put students in good stead before they enter their more intensive and long-term 4-month research block.
3. Four-month research block
In the latter part of their 2nd year or their 3rd year, our medical students are required to make a full-time commitment of four months to conducting research as part of a mentored learning experience, carrying out an in-depth investigation of a problem or issue that is empirical and hypothesis-driven. There are four different times at which students can schedule their research blocks to fulfill this requirement. Students are assisted by OMSR, the deans of their academic societies, the Vice Dean of Research, and other faculty members in selecting appropriate mentors, matching their research interests to appropriate investigators in laboratories or clinics. The sites for their research may be at CWRU School of Medicine or any of its affiliated institutions, which includes a prestigious private clinic with an active and wide-ranging research program, an academic medical center, a large urban hospital with a significant needy clientele, and a Veteran Affairs medical center. With all of these sites available for research, there is no shortage of appropriate research opportunities for students that provide a good match with student interest and background. Students may also opt to work in a lab or clinic outside of CWRU School of Medicine, given that they fulfill the requirements of having their research proposal approved and of naming an appropriate co-advisor affiliated with CWRU SOM.
As with summer research, we ensure that the student involvement in the research is high-level and meaningful, but their role now requires more autonomy in shaping the inquiry, responsibility in generating results, and accountability in creating intellectual products (especially a research summary that will usually become the basis for their medical thesis). Generally speaking, students affiliate themselves with principal investigators whose research activity is ongoing or have a project that is soon to be launched, complete with institutional review board (IRB) approval. Students work with their prospective mentors to carve out a set of questions or hypotheses in which they have ownership, but which also meshes with the larger research agenda of the laboratory or clinic. Working under the guidance of their research advisor, students craft a proposal that lays out the importance of the question or issue that they intend to investigate; clearly and explicitly defines the hypotheses or questions to be tested; and specifies the methods that they will employ to test these hypotheses. They must also conduct a preliminary literature review to gain an understanding of the importance of the topic, what has already been established in the field, and how their own research question relates to other open questions in the domain. They conclude the proposal by describing in detail the specific roles and responsibilities that they will fulfill in carrying out the research. Since they have moved along a developmental trajectory in building their research knowledge and skills, we expect a more detailed research proposal than is expected for students conducting summer research after their first year of medical school.
The research performed for the 4-month research block must meet certain criteria. Foremost, the research must be hypothesis-driven: there must be a hypothesis (or set of hypotheses) that is empirically testable, and all other aspects of the research must be aimed at investigating the hypothesis. Students must be working with original, largely unprocessed data. While the research fits in with the aims of the laboratory or clinic in which they are conducting their research, they must find a niche for themselves within this work and take ownership over questions that will drive their own investigation. This requires that students negotiate their research focus with their prospective mentors before starting their research block. Students must determine that the institutional review board (IRB) approval will be in place in a timely manner, so that their work during the block is not impeded. Occasionally, we have students who wish to pursue an original research idea. If this is the case, we fully support the student, but make him or her aware that they will need to start planning for their de novo research project well before the start of the 4-month block, that they will need to find a mentor who sponsors them in the project and is willing to provide intensive mentorship and guidance as they formulate and implement the project, and that they will need to work with this mentor to put in place IRB approval before the start of the block. Such highly individualized research will likely require time beyond the 4-month block to finalize the data gathering and analysis.
At the conclusion of the block, students are required to submit a summary of their research. This summary can be seen as a working draft of the medical thesis that they are required to submit in order to graduate in the 4th year of medical school. Some students opt to continue the research endeavor that they began in their research block in order to gather more data, complete the analysis of data collected, or work with their mentors to put their research into a publishable form. One-month research electives are available for them to complete their research, if necessary.
4. Medical thesis
Typically, the work that students carry out in their 4-month research block becomes the basis of their medical thesis. The format and content of the medical thesis should emulate an article as it would appear in a peer-reviewed journal in their field. Thus, the term “thesis” may be a misnomer, since it is unlike a thesis one would write for graduate school, but the term has become entrenched at the medical school (“research report” might be a better term).
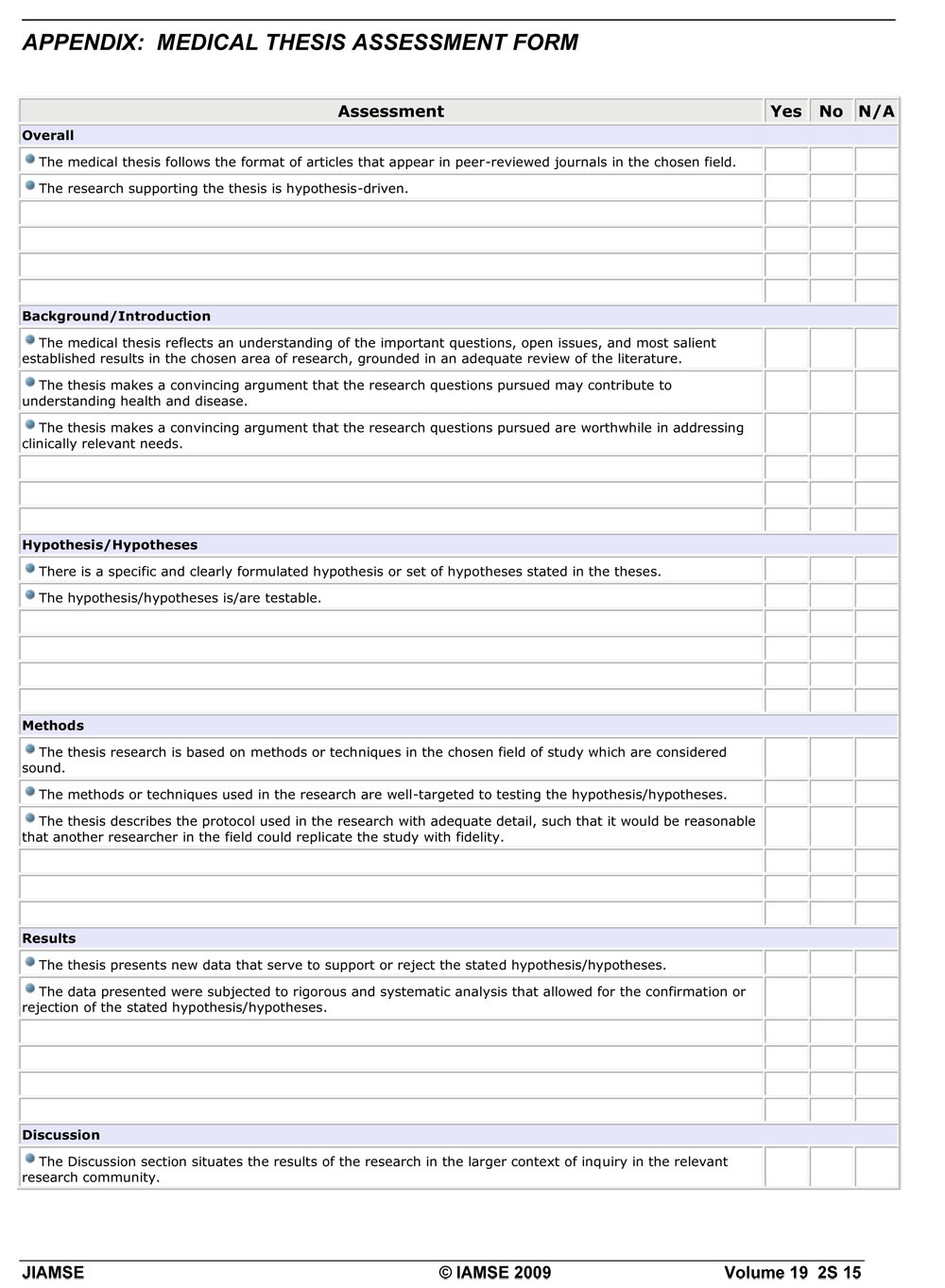
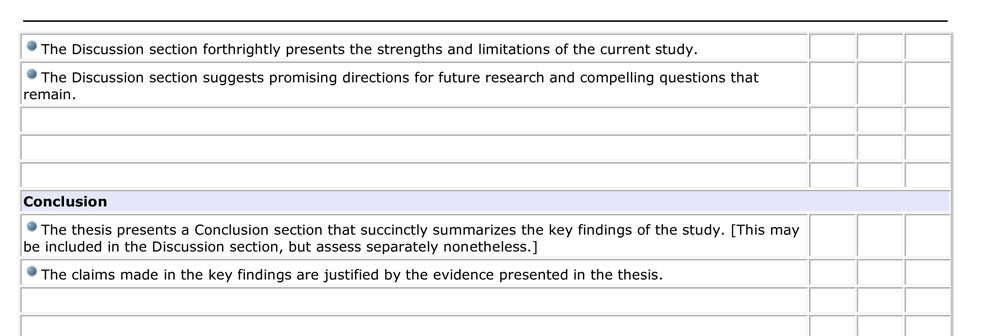
At this point in the student medical school career, there should be no surprise that the thesis must be based on empirical research that is hypothesis-driven. The intent of this learning experience is to simulate a peer-review process for students, granting them a sense of what it is like to publish research in the field of medicine. We have assembled a medical thesis review committee, composed of researchers with a range of expertise to match the variety of medical thesis topics that students submit, who apply criteria that are the usual criteria one would find applied in selecting articles for any peer-reviewed journal. In general, these criteria track the key sections of a prototypical journal article: 1) is the overall research hypothesis-driven?; 2) are clear and testable hypotheses presented?; 3) are replicable methods described that are well-targeted to testing the hypotheses?; 4) do the results presented serve to confirm or reject the hypotheses?; 5) is there a forthright discussion of the strengths and limitations of the methodology used?; and 6) are the key findings supported by the evidence in the report? (The appendix presents in detail the criteria that our reviewers use.)
There are students who do, in fact, work with their mentors to publish an article in a journal. Naturally, this is encouraged; we see such student research productivity as a key indicator of the success of our medical student research program. If students publish their research as a co-author, they must establish that they had a significant role in the authorship of the manuscript and their mentor needs to attest to this. It is also possible for students to submit a thesis that is a product of research effort conducted while in medical school but not connected to their research block project. The “peer reviews” provided by faculty are shared with students, and they are given a chance to revise their thesis to meet the requirements of the thesis.
5. Further opportunities for research: Year-off opportunities, dual degree programs, and options for research electives
We have students who become so engrossed in research that they decide to pursue a year-off to delve deeply into a problem or issue of great interest to them. Our program allows for students to take a year-off, and OMSR works with students who are interested in participating in year-off research identify and compete for funding opportunities, such as fellowships from the Howard Hughes Medical Institute, Sarnoff Foundation, the Doris Duke Foundation, or Fogarty International.
Finally, students may pursue a dual degree option to expand their opportunities to pursue an area of research interest in greater depth and deepen their skills and understanding in a specialization. These dual degree programs include an MD/MA in Bioethics, an MD/MPH, an MD/MS in Anatomy, an MD/MS in Biomedical Engineering, and an MD/MS in Biomedical Investigation.
Lessons Learned and Future Directions
The research component of our curriculum pitches a student forward on a developmental trajectory, where the student moves from peripheral participation in a community of researchers to increasingly active, complex, and autonomous roles in such communities as they take on more challenging research activity and further develop their research skills and knowledge [3, 4]. We have faced a number of challenges in helping students move along this trajectory; examining these challenges will inform our improvement efforts as we act on enhancing student preparation for productive and meaningful engagement in their research block.
First, the Foundations of Medicine and Health curriculum needs to be strengthened to address difficulties that students often encounter as they formulate their research proposals for their summer or research block experience. More attention will be given to developing student skills in generating and formulating hypotheses; in bolstering their understanding of appropriate statistical measures and how to interpret them; and in increasing their ability to critique – and even rethink – the methodologies they employ in carrying out their research. This is especially vital for those students who have not conducted research previous to matriculating at our medical school.
It is hoped that strengthening these aspects of our curriculum will reduce the occurrence of two common problems that we see in reviewing research proposals: 1) failure to clearly and explicitly articulate hypotheses; and 2) omission of a detailed description of the student specific roles and responsibilities in carrying out the research (some students only provide highly generic language about how research is performed in the clinic or laboratory).
As the students move into their research block, the mentorship and support that their principal investigator provides to them becomes critical. We are looking at ways to bolster the assistance and support we provide to mentors, and to improve communication of the expectations that hold for their work with students, articulating clear roles and responsibilities for them. Student research block experience is viewed as a mentored learning experience, and the meaningfulness, engagement, and intellectual substance of the experience depends critically on the mentor skills in modeling and coaching research thinking and activity, as needed for the student. Mentors need to work with students to heighten their intellectual ownership of the work being performed, prompting them to pose worthwhile questions, think critically about methodologies, improve protocols, analyze and represent data, interpret results, consider alternative explanations of data, and learn how to communicate their research to others. Effective mentors look for ways to heighten student intellectual engagement and to help students take advantage of multiple opportunities to present and publish their results (e.g., attending conferences, co-writing articles, submitting abstracts, writing grant proposals, documenting IRB processes).
In addition to the support of mentors, we are planning to put in place other supports that will better prepare students for the research block. We wish to help students access resources in statistical and research design consultation as they plan for, implement, and evaluate the results of the research performed during their block. We want to provide opportunities for students to “workshop” their proposals before entering the block, speaking with other students and faculty experienced in research methodology to think more deeply about their hypotheses and the research designs to test them. During the block, we are planning workshops targeted at high-priority skills and processes in research activity (IRB process/approval, writing of proposals or structured abstracts, effective poster design, etc.) In this way, we want to create an even stronger support system to better ensure that all students in our medical school curriculum have a meaningful, high-quality mentored learning experience for their research block. Such a support system will help students integrate the research block experience more effectively and coherently with the rest of the medical school curriculum. This, in turn, will promote the shift in attitude we wish to see in students: an attitude where clinical practice is not seen as divorced from research, but part of the continuum of reflective practice that should pervade inquiry, whether it is situated in a clinical setting or a research setting.
The culmination of this developmental trajectory in research skills and knowledge comes with the writing and submission of the medical thesis. Here, we wish to help students work on clearly stating their focus and research question, engaging in an adequate critical discussion of the strengths and weaknesses of the study methods, and offering conclusions that are properly qualified in their scope given the evidence gathered and analyzed. We hope the strengthening of the research component of the curriculum, careful mentorship, and the provision of wider support systems will better ensure that all students are producing high-quality theses meeting or exceeding the criteria listed in the appendix.
Our medical thesis reviewers need to be clear that their function, at the point when the thesis is submitted (in early January of the student’s fourth year of medical school) is to provide a “peer review” of the thesis, rather than mentorship. Our medical thesis reviewers, especially those who are not M.D.s but are Ph.D.s, need to learn to recognize that this thesis differs from those that would be submitted by students working on a master or doctoral degree in basic science programs. They need to adjust their expectations in evaluating the research reports of our medical students, submitted as medical theses.
Finally, for those students submitting articles that they co-authored with their PIs, we need to make clear that they had substantive roles in writing the manuscript, establishing that it is legitimate for them to claim a significant portion of the work as their own.
CONCLUSION
The structured research activities in which students are engaged throughout their medical school career at CWRU SOM are aimed at cultivating the reflective habits of mind associated with professionalism in medicine. Increasingly, students over the course of their medical school career at CWRU SOM are engaged in more complex and self-directed research efforts that draw them from the periphery of working in communities of research and inquiry into the core of such communities. It is in this activity that students see modeled, and put into action, reflective practice, practice that integrates reflection and action as aspects of the same professional orientation. This reflective practice is reinforced and extended by other aspects of the medical student curriculum, including the dialogue and reasoning centered on the cases that students work through in their problem-based learning sessions (a key part of our curriculum) and the portfolio processes in which they engage.
It has been argued in this manuscript that the habits of mind so intimately bound up with medical professionalism are precisely those habits of mind fostered in the activity of research. It is the aim of CWRU SOM research component in the curriculum to provide the opportunities, structure, and environment for its medical students to engage in meaningful research, with the ultimate hope of developing students into lifelong learners inured to these habits of minds. In this way, our medical students will emerge from their medical school experience with a clear sense of what it means to be a physician-scholar, a professional committed to ongoing cycles of reflection and action in their careers and to continual, systematic inquiry, moving toward more structured research activity in their practice as appropriate and enriching, but always engaged in reflective practice.
REFERENCES
- Professionalism. Academic Medicine. 2007; 82: entire issue 11 (Whitcomb ME, editor).
- Shön, D. The reflective practitioner: how professionals think in action. New York, NY: Basic Books, 1983.
- Lave J, Wenger E. Situated learning: legitimate peripheral participation. Cambridge, UK: Cambridge University Press; 1991.
- Wenger, E. Communities of practice: learning, meaning, and identity. Cambridge, UK: Cambridge University Press; 1998.