ABSTRACT
Growing attention to end-of-life care has fostered innovation in medical education. We describe an effective model to introduce third-year medical students to principles of end-of-life care, and spirituality and faith traditions in the care of the dying. Many aspects of the curriculum are adaptable for use at other medical schools.
Growing attention to end-of-life care has inspired curricular innovation and change in medical education. Traditionally, medical school curricula advanced curative principles of care. Over the past decade, health professionals, patients, and families have recognized the need to improve care during the final stages of illness. This movement resulted in calls to improve physician education in end-of-life care, including the Institute of Medicine’s seminal 1997 report, Approaching Death.1
To ensure U.S. medical schools address end-of-life care, the Liaison Committee for Medical Education (LCME) “Functions and Structure of a Medical School” provides the following mandate:
- ED-13 Clinical instruction must cover all organ systems, and include the important aspects of preventive, acute, chronic, continuing, rehabilitative, and end-of-life care.2
Medical schools have responded by introducing coursework and experiential learning activities. A 2004 review of teaching and learning in palliative care documented considerable variation in curricula and methods.3 Examples include an intensive, one-day, classroom-based intervention; an interdisciplinary workshop; third-year clerkship experiences; and a student-initiated, elective preceptorship.4-7 In this paper we describe another variation, an innovative, required course to address end-of-life care and human spirituality.
In 2003, Creighton University School of Medicine introduced Dimensions of Clinical Medicine (DCM): Palliative Care. This half-day course module is required for third-year medical students. The module is part of the Dimensions of Clinical Medicine interclerkship course, and occurs during students’ third clerkship. DCM began in 2002-2003, and has proved effective for presenting clinically relevant content to third-year students.8 Consistent with adult learning principles, the course offers students knowledge and skills when they are most likely to need them, i.e., during their first clinical year.9 The palliative care module was revised in 2006 to also explore how faith and spirituality affect perceptions of death and care of the dying. The course goals reinforce our medical school’s institutional values. As a Jesuit Catholic medical school, Creighton University School of Medicine is committed to providing compassionate care of the whole person. This value, known as cura personalis, is a hallmark of Jesuit education. Cura personalis emphasizes concern for the whole person and dedication to promoting human dignity.10
The course is organized around seven objectives (Table 1). The session begins with an overview presented by the Medical Director of Palliative Care Services for the region’s largest healthcare system. The presentation reviews the historical origins of palliative care, highlights differences between curative and palliative care, and describes the physician’s role in palliative care. Next, students view “The Way We Die: Listening to the Terminally Ill,” an award-winning video featuring interviews with patients, family members and doctors.11 Afterwards, the hospital chaplain facilitates a reflection on the dying.
- Table 1. Dimensions of Clinical Medicine: Human Spirituality, Palliative, and End-of-Life Care Learning
After participating in the Dimensions of Clinical Medicine Human Spirituality, Palliative, and End-of-Life Care sessions, students will be able to:
- 1.Discuss 3-4 objectives of palliative and end-of-life care that might guide a hospice or healthcare team.
2.Describe examples of effective patient and family involvement in end-of-life decision-making.
3.Paraphrase 3-4 common questions about palliative and end-of-life care asked by patients and their families.
4.Describe examples of different faith traditions and propose how these might affect the needs of patients and families.
5.Discuss the role spirituality can play in the life of a person receiving palliative or end-of-life care.
6.Generate a list of 3-4 palliative and end-of-life care resources for student and patient use.
7.Describe the life cycle and explain how death and dying are a part of the life cycle.
The next activity is the Faith Traditions Panel. The panelists, representing multiple faiths, describe beliefs and customs and their significance to patients, families, and health professionals. Two small group sessions follow, and panelists serve as facilitators. The course concludes with the session “The Impact of Spirituality upon the Death of a Child” presented by a pediatric oncologist. Following the course, students critique resources such as publications or multimedia presentations. The objective is to ensure students reflect on the course and the questions that patients and families pose about end-of-life care.
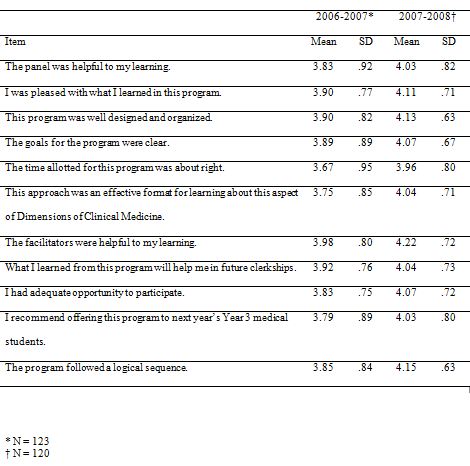
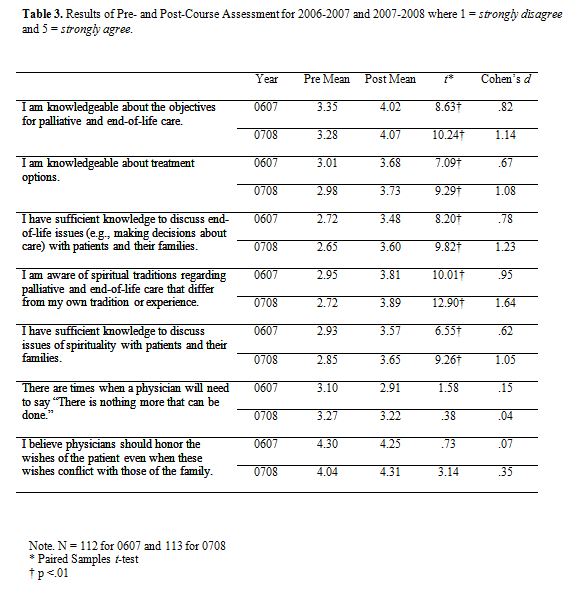
To investigate the effectiveness of the revised course, we examined data from evaluations and pre- and post-course assessments. The Creighton University IRB granted exempt status for this investigation. We used a web-based education management tool to administer the 12-item course evaluation (Table 2). The seven-item pre- and post-course assessment was constructed for the course. Five items asked students to self-assess their knowledge of covered topics. Two items assess student attitudes toward two fundamental principles of palliative care. Both instruments included open-ended questions to probe for prior knowledge and experience and inquire about topics of interest (Table 3).
For both academic years 2006 and 2007, students indicated satisfaction with the revised curriculum and overall experience with the course (Table 2). The highest rated item was “The facilitators were helpful to my learning” (3.98, 4.22). The lowest rated item, “The time allotted for this program was about right” (3.67, 3.96), may be better understood by examining student comments. Some noted that valuable discussions were curtailed due to time constraints, and others requested more time with the faith traditions panelists. For both years, the discussion of religious and cultural issues was the most frequently cited topic in evaluation comments.
- Table 2.Mean ratings of course evaluation data for 2006-2007 and 2007-2008 where 1 = strongly disagree and 5 = strongly agree.
We compared results from the pre- and post-course assessments using paired-samples t-tests. We detected statistically significant gains in student knowledge after completing the session (Table 3). Learning outcomes measured by the pre- and post-course assessment were analyzed using Cohen’s d statistic to calculate the effect size (ES).12 For this matched pair analysis, the effect size was calculated by using the t score and dividing it by the square root of the degrees of freedom.13 By convention, an ES of 0.2 indicates a small, 0.5 a medium, and 0.8 a large effect. For both years, several items produced a large effect, with the largest effect detected for the items “I am aware of spiritual traditions regarding palliative and end-of-life care…” (ES .95, 1.64); “I am knowledgeable about the objectives…” (ES .82, 1.14); and “I have sufficient knowledge to discuss end-of-life issues…” (ES .78, 1.23).
We were pleased that students reported gains in their knowledge for all learning objectives, including the two new objectives addressing faith traditions and human spirituality. We were interested to observe that some student’ attitudes toward the role of a physician with a dying patient changed after this brief course. We hypothesize that the non-significant changes, where items had an ES less than .20, reflect students’ prior knowledge and beliefs.
Students were satisfied with the course, and in particular, with presenters and facilitators. This is important because the presenters were selected by the course directors for their expertise and experience. With one exception, all were invited from outside the university. Positive student feedback is valuable for course planning and also for sharing with the presenters who take time from their professional practice to participate. Student’requests for additional small group time suggests they find the course content interesting and deserving of extra time for discussion.
Two limitations should be noted. First, data are available for two years only. Although evaluation data from previous years are available, the curriculum changed after 2005, impeding meaningful longitudinal comparisons. Second, the pre- and post-course assessment instrument has not yet been formally validated.
The DCM: Human Spirituality, Palliative, and End-of-Life Care course differs from other approaches described in the literature. This course is required, occurs during the third year of medical school, addresses spirituality, and incorporates small group discussions and a panel presentation. Unlike many courses that draw upon psychiatry faculty, this course includes presenters with expertise in palliative medicine and pediatric oncology. In addition, respected community members are invited to participate.
Our findings suggest that this course is an effective model for teaching medical students about end-of-life care and human spirituality. The curriculum successfully introduced students to new perspectives and accounted for significant knowledge gains. Changes in student attitudes were modest but suggested the course provided new information that fostered reflection on current beliefs. We believe many aspects of the curriculum are adaptable for use at other medical schools.
REFERENCES
- 1.Institute of Medicine. Approaching death: Improving care at the end of life. Washington, DC: IOM, 1997.
2.Functions and structure of a medical school: Standards for accreditation of medical education programs leading to the M.D. degree. (http://www.lcme.org/functions2007feb.pdf). Accessed October 15, 2007. Liaison Committee on Medical Education, 2004 (with updates as of February 2007).
3.Lloyd-Williams, M., and MacLeod, R.D. A systematic review of teaching and learning in palliative care within the medical undergraduate curriculum. Medical Teacher. 2004; 8:683-690.
4.Clay, M., Jonassen, J., and Nemitz, A. A one-day interclerkship on end-of-life care. Academic Medicine. 2001; 76:517-518.
5.Latimer, E.J., Deakin, A., Ingram, C., O’Brien, L., Smoke, M., and Wishart, L. An interdisciplinary approach to a day-long palliative care course for undergraduate students. Canadian Medical Association Journal. 1999; 161:729-731.
6.Leslie, B., Adams, L., and Kutner, J.S. Integrating and end-of-life curriculum into the Internal Medicine clerkship. Journal of Palliative Medicine. 2002; 5:752-753.
7.Taylor, L., Hammond, J., DiCarlo, R., Karabatsos, G., and Deblieux, P. A student-initiated elective on end-of-life care: A unique perspective. Journal of Palliative Medicine. 2003; 6:86-91.
8.Sakowski, H.A., Markert, R.J., Jeffries, W.B., Coleman, R.M., Houghton, B.L., Kosoko-Lasaki, S., Goodman, M.D., Rich, E.C.: Dimensions in Clinical Medicine: An interclerkship program. Teaching and Learning in Medicine. 2005;17(4): 370-375.
9.Knowles, M.S. The adult learner. Woburn, MA: Butterworth-Heinemann, 1988.
10.Traub, G.W. Do you speak Ignatian? A glossary of terms used in Ignatian and Jesuit circles. Cincinnati, OH: Xavier University, 2004.
11.“The Way We Die: Listening to the Terminally Ill,” Jonathan Mednick. Fanlight Productions. 1995.
12.Cohen, J. Statistical power analysis for the behavioral sciences. New York: Academic Press, 1977.
13. Rosenthal, R., and Rosnow, R. Essentials of behavioral research: methods and data analysis. New York: McGraw Hill, 2008.