ABSTRACT
Purpose: The purpose of the project was to examine the feasibility and acceptability of a technology-based geriatric training program for third-year Family Medicine (FM) students.
A one-group, pre-post intervention study was conducted between 2004 and 2005. Participants were 24 third-year medical students , assigned to rural FM practices, in which at least 30% of the patients were 65 years of age or older. Students were taught to access Geriatrics at Your Fingertips and other geriatric assessment tools, using internet and Personal Digital Assistant (PDA)-based formats. Case studies were reviewed to illustrate their utility. Students were emailed weekly for progress reports and electronic logs of their older patient encounters. Students completed baseline questionnaires to assess their familiarity and comfort level using internet and PDA. After the rotation, they completed questionnaires about the helpfulness and feasibility of using this educational technology.
At baseline, all students felt confident using the web and 96% felt confident using a PDA. These results remained unchanged after the rotation. After the intervention, 96% used the web to access medical information, and 100% used a PDA. Almost all of the students reported that geriatric assessment modules on the PDA enhanced their diagnostic and assessment skills for older patients; while 46% were undecided or felt that the web-based modules were not feasible in a busy rural practice.
Technology-based geriatrics education in rural FM practice is feasible and acceptable to third-year students. Geriatric assessment modules on the PDA were perceived to enhance older adult encounters at the point of care.
INTRODUCTION
An August 2000 survey of course and clerkship directors revealed that the current University of Alabama School of Medicine (UASOM) curriculum includes only about 24 hours (or 1 In addition, 30-40% of senior medical students completing the Association of American Medical Colleges 2000 Medical School Graduation Questionnaire indicated that instruction devoted to long-term care, geriatrics, and palliative care was inadequate. Few practicing physicians are prepared to manage geriatric syndromes and diseases associated with aging or to recognize the heterogeneity of function and physiology in normally aging adults. In addition, demands on medical school faculty for increased productivity and greater reliance on community-based preceptors to provide outpatient clinical learning opportunities pose formidable challenges as medical schools strive to fulfill the requirement of the Liaison Committee on Medical Education that all medical students receive an equivalent educational experience and achieve the same core competencies.1
In response to this growing need, we integrated geriatric education into the Family Medicine (FM) clerkship, a required four-week experience taken during the third year of the UASOM curriculum. The purpose of the clerkship is to provide third year medical students with an understanding and awareness of the broader social context of health in the community by focusing on health-related issues of Alabama’s rural population. Most of the practices in the rural communities where the medical students rotate are distant to hospitals and do not have immediate access to emergency services or other medical resources. Medical libraries and frequent interaction with specialists are typically not available in these remote areas, which place great demands on the family physician scope of knowledge. Medical students rotating through FM in rural sites therefore encounter challenging cases about whom they may wish to obtain more information than is typically available. Thus, this clerkship represented an ideal opportunity to employ distance-learning techniques, based on principles of geriatrics assessment. The education program we developed was designed to provide students with resources to assist in the diagnosis and treatment of geriatric patients.
The primary aim of this educational project was to evaluate the feasibility and acceptability of PDA and web-based technology as a diagnostic and management tool for medical students caring for older adults in rural settings. Therefore, we made geriatric educational modules available through Personal Digital Assistants (PDAs) and laptops with internet access, to provide the students with the aging-related medical references and information they currently lack in these outlying areas. With the use of technology at the point of care, we implemented a training program to improve geriatric education and ensure that all students had consistent exposure to important geriatric issues.16
MATERIALS AND METHODS
This project was approved by the institutional Review Board for Human Use.
Participants and Setting
Between November 2004 and August 2005, we recruited 24 third-year medical student volunteers who were assigned to preceptors with large geriatric patient populations (i.e.<30%) during their FM clerkship in rural sites. All students received lap-tops and PDAs and a seventy-five dollar monetary stipend for their participation in the study. A letter was sent to the FM preceptors in the rural sites requesting their permission to allow the use of PDAs and laptops by the medical students assigned to their practices. References for the geriatric assessment materials were made available to the preceptors upon request.
Letters were also sent to potential medical student research participants. The letters specified the monetary compensation for participation in the study and the meeting time and location during Orientation Day for the FM clerkship.
On Orientation Day, the Principal Investigator (PI) conducted a formal presentation to all students in the clerkship regarding the purpose and procedures related to the study. They were made aware that participation in the study was strictly voluntary and would not affect their grades. After this, the students were given consent forms, and if they were agreeable with the terms of the study, the PI enrolled them for the 4 weeks of clerkship. There were no exclusion criteria.
Assessments
On Orientation Day, student participants recorded their age, gender, prior medical background, and previous PDA and/or web exposure. At the end of the clerkship, the feasibility and acceptability of PDA and web-based technology was evaluated using self-administered questionnaires. Responses to the questionnaires were tabulated and summarized using descriptive statistics.
Educational Intervention
All students were provided with laptops and PDAs (2005 version, Palm Operating System OS) for the duration of the study. We evaluated the student skill level in using the internet and PDAs and as needed, provided additional training. Specifically, we taught the students to access the print version, the web version and the PDA version of Geriatrics at Your Fingertips (GAYF) (2004-2005 version, American Geriatrics Society) thereby allowing access to information about diagnosis, evaluation, and treatment of the most common geriatric syndromes at the bedside.2Assessment instruments to evaluate the patient memory, mobility, mood, pain intensity, and function were also made available at the point of care. Additionally, the students were taught to access Epocrates3 (2004-2005 version) on their PDAs. Epocrates is a software program with over 3,000 brand and generic drugs. The students accessed drug dosing, potential drug interactions, and drug pricing using this program.
Our educational objectives encouraged the students to use the GAYF, which includes information about age-related physiologic changes, formulas, and specific assessment instruments for disorders affecting the aging population. In the event of technological failure, the medical students had GAYF in book format. We worked closely with the University’s Office of Curriculum Development and Management and the Department of Information Technology, which assigns all students internet-accessible e-mail accounts in their freshman year. We communicated closely via e-mail with the students to answer questions, monitor their progress, and guide them through potential difficulties with software and/or hardware use.
Once GAYF was loaded onto PDAs and the lap-tops, a feasibility study of our information technology was conducted: Three case studies on dementia, depression, and renal failure from the Geriatrics Review Syllabus that utilized assessment instruments to evaluate geriatric syndromes were selected.4 The Syllabus is a publication of the American Geriatrics Society with 59 chapters and clinical cases, covering the prevailing management strategies for the older adult. Small group discussions were then held to discuss the case studies that utilized assessment instruments available thru GAYF.
RESULTS
Characteristics of the Student Participants
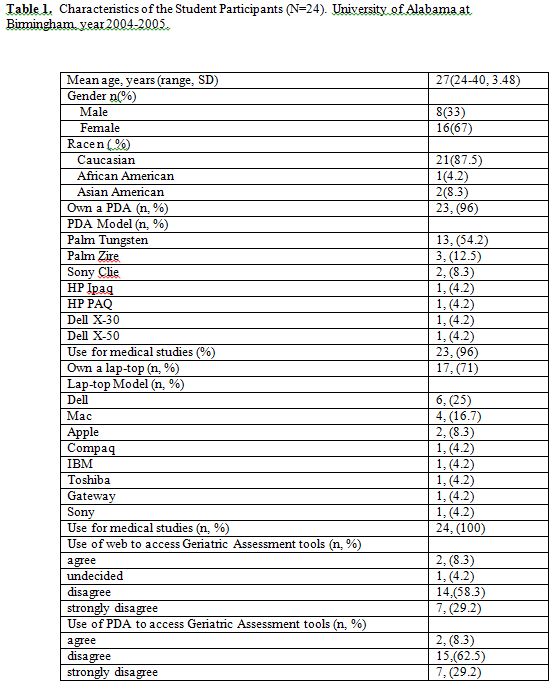
Most participants were Caucasian females between the ages of 24-40 years (Table 1). Ninety-six percent of the students owned a PDA with 54.2% of them owning a Palm Tungsten. Seventy-one percent of the students owned a lap-top, of which 25% were a Dell brand. More than half of the students did not use the web or the PDA to access geriatric assessment tools before the intervention (Table 1).
Utilization and Feasibility of Medical Technology
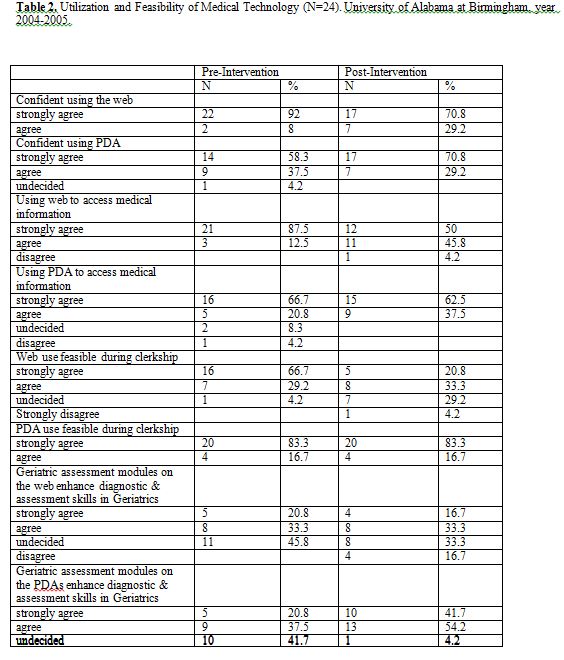
We used a 5-point Likert scale to compare the pre- and post- attitudinal responses of the participants before and after the FM clerkship. At baseline, all students felt confident using the web and 96% felt confident using a PDA, and this was unchanged after the rotation (Table 2). Before the intervention, 87.5% of the students strongly agreed that using the web to access medical information was feasible. However after the FM rotation, only half the students strongly agreed that using the web to access medical information was feasible and practical. Before the intervention, more of the students stated that they preferred to use the internet rather than the PDA to access information. After they returned from their clerkship rotations, they all indicated a preference for using the PDAs to access aging-related medical information, and PDA use for this purpose grew by 12.5%.
Before the intervention, almost all of the students believed it was feasible to use the web to access medical information during clerkship training and more than half of them believed the assessment modules on the web enhanced their diagnostic and assessment skills pertaining to their older adult patient (Table 2). After our intervention, about half believed it was feasible to use the web to access medical information primarily because it proved cumbersome to carry the laptops from room to room. At baseline, all students believed it was feasible to use the PDA to access medical information during clerkship training, and this was unchanged after the rotation. In contrast, the number of students who believed that the assessment modules on the PDAs enhanced their skills increased from 58% to 96% after the rotation. Therefore, the students were better able to appreciate the value of geriatric assessment modules on the PDAs rather than on the internet after their rural FM rotation.
Evaluation of Field Experience
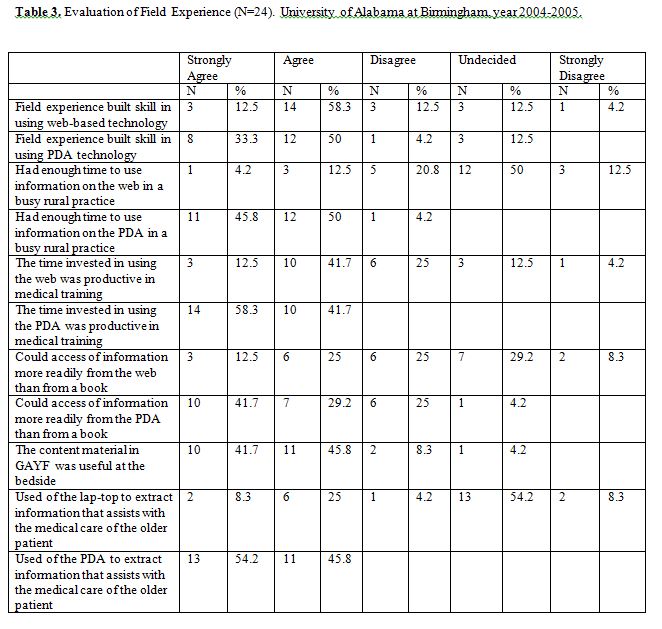
The majority of students felt that the educational experience built their skills in using web-based (71%) and PDA-based technology (83%) (Table 3). Few felt they had enough time to access information on the web in a busy rural practice, while all but one reported sufficient time for the use of PDAs (Table 3). The majority noted that the time invested in using the web was productive in their medical training, while all of the students felt that using the PDA was productive during their clerkship. (Table 3). After the intervention, about a third of the students could more readily access information from the internet than from GAYF in the book format, while 71% felt similarly about their PDAs . Most of the students (87%) indicated that the content material in GAYF was useful at the bedside. Approximately, one-third of them used lap-tops to extract information to assist with the medical care of their older patients, and they all used PDAs. No students chose the web as the most effective tool to access GAYF.
Informal Qualitative Reports
The students reported informally that the size and immobility of current internet-based technology made it difficult to use. They recommended that the equipment be made more compact and wireless. The students noted that they did not have time to sit at a computer in a busy practice, and that it was inconvenient to carry around a lap-top all day. They felt that wireless internet access in the office and hospital could increase the feasibility of using computers in those settings. They also believed that a high-speed internet connection rather than dial-up computer access at the bedside would increase efficiency. They noted that having a PDA that could access the web through Wi-Fi would enhance their utility and that access to a variety of good, simplified PDA software would be essential early on in their training, when thinking through the patient differential diagnosis is challenging. Our discussions of the data also represented opportunities to demonstrate the wide spectrum of geriatric issues seen in FM. The chief complaints, for which students consulted GAYF, included arthritic, cardiac, pulmonary, dermatologic, endocrine, neurologic, psychiatric, and urologic disorders.
DISCUSSION
In the last two decades, a number of reports have recommended that medical schools incorporate educational technology into their teaching programs. In 1992, the Report Writing Committee of the Association of American Medical College’s Assessing Change in Medical Education – The Road to Implementation Report (AAMC’s ACME-TRI Report) suggested that medical schools improve faculty knowledge about the use of educational technology, provide more and better organized computer software resources to facilitate student learning, and develop organizational structures that promote the use of educational technology.5 However according to a 1998 analyses, U.S. medical schools have made limited progress in accomplishing these goals.6
The increasing use of community clinics and hospitals for educating medical students has created obstacles to delivering a uniform curriculum to learners. Internet-based learning modules may represent a means to address this problem. The use of computer-assisted learning enables all students to be taught the same material in their own time and at their own pace. Computer-assisted learning programs have also been shown to be efficacious in teaching geriatrics content to undergraduate medical students.7,8
According to a recent survey of 834 U.S. physicians, about 26% used handhelds in 2001, and an estimated 50% would use the devices by 2005.9 Practitioners use these devices to access drug dosing, costs, and databases with information on potential adverse drug reactions among medications, as well as health plan guidelines, protocols, and calculations that are useful at the point of care.10,11
Recognizing that familiarity with information technology will be as important to the future physician as knowledge of the path physiology and treatment of common diseases, many medical schools in the United States, including Wake Forest University, and Stanford University are providing their undergraduate students with handheld computers.12,13
Medical students are using handheld computers to keep track of clinical encounters and facilitate evidence-based decision making.14 To meet the changing information needs of their trainees, medical training programs are integrating handheld computers in their curricula. Given the growing volume of medical information and the increasing expectation for practitioners to adhere to standards of evidence-based care, physicians and trainees increasingly require ready access to medical information at the bedside. The appeal of the PDA is that it can function as a compact, portable medical information resource that can be accessed at the point of care. Moreover, it can be easily updated to incorporate emerging research and evolving clinical practice guidelines.15
Handheld devices are widely used in FM residency programs in the United States. Studies indicate that PDAs are being used for some purpose in two thirds of family practice residency programs, and their use is mandatory in 30% of them. Although they were designed as electronic organizers, in family practice residencies they are used as medication reference tools, electronic textbooks, and clinical computational programs.16 PDAs are portable, relatively inexpensive, and have the ability to interface with other electronic devices, including desktop computers. The adoption of this technology may influence how we teach or train medical students and residents to appropriately access and use available up-to-date clinical information to improve patient care.17
Readily available patient-specific or application-specific information at point-of-care allows for more complete and accurate information for the patient encounter. Drug dosages and clinical computational formulas that, prior to the advent of handheld computers, were accessible only by pencil-and-paper methods are immediately available on handheld computers, reducing potential for errors or outdated information. Likewise, applications for up-to-date clinical information from electronic textbooks and on-line sources encourage users to continue as lifelong learners.18,19
CONCLUSION
This study provides preliminary evidence suggesting that PDA utilization to enhance geriatrics education in rural Family Medicine practice sites may be most useful. Several limitations of our work deserve consideration. Our study cannot assess whether the use of technological tools enhanced student proficiency in geriatric care and points to the need for follow-up studies using a pre-post randomized control study design to assess the specific impact of technology-based intervention on clinical competence. Future work should focus on evaluating the impact of the intervention on student acquisition of geriatric knowledge. We experienced difficulties tracking time and movements of the users and relied on self-identification of resource utilization. Although our sample size of 24 students is too small to assess improvements in geriatric knowledge, we were able to demonstrate that technology-based geriatrics education in rural FM practice sites is feasible and acceptable to third-year students and that students perceived that using geriatric assessment modules on their PDAs enhanced their older adult encounters at the point-of-care. We recognize that utilizing teaching tools for medical training does not substitute hands-on teaching skills taught by preceptors in the community. Our hope is to utilize teaching resources to augment and standardize some elements of clerkship training in geriatrics while stimulating self-directed learning.
Medical education technology for students that is highly mobile, and allows much of their work to be done off-campus, is one potential future direction. Mobile learning refers to the use of mobile, hand-held electronic devices for medical education. These devices could include PDAs and cellular phones. Mobile learning is still a developing area, but it already offers many advantages. Mobility, portability, low pricing, and small size are all advantages of mobile learning in medical education. Medical students can access medical information without being tied to a specific location, and the device can easily be dropped into a pocket to free both hands. At the present time, PDAs are being phased out in favor of devices that combine cell phone and PDA functionality, as well as other functions such as video camera and web access.16
The iphone is the latest mobile device that has recently appeared in stores. The newest iphone has a built-in GPS chip, iPod, high-speed mobile wireless web browsing, e-mail, telephone, and PDA capabilities all in one device. However, one needs to have a contract with a specific telephone company to use this latest version of mobile learning. Technology will simplify life for health professionals as the cost to purchase and utilize mobile devices become more affordable for students and practitioners in medical education.
ACKNOWLEDGEMENTS
The authors wish to thank UAB’s Department of Family Medicine, specifically Dr. Michael Harrington and Dr. Tamela Turner, who allowed access to the FM students. The authors also wish to thank Mr. Jeffery James and Dr. Phillip Thornton for loading Geriatrics at Your Fingertips & Epocrates onto PDAs. Mr. James works in the Department of Family Practice at UAB and provided technological support and assisted in the initial PDA and laptop programming. Phillip L. Thornton, Ph.D., R.Ph. was an Auburn University Assistant Professor, who worked closely with me at the Spain McDonald clinic training pharmacy students. Dr. Thornton is highly skilled with PDA and Internet applications. The authors also wish to acknowledge support from the Southeast Center of Excellence in Geriatric Medicine whose generous funding allowed for protected time and resources to conduct this study.
There are no conflicts of interest for the authors. The results of this research were presented as a poster at the 45th annual Association of American Medical Colleges meeting in 2006.
REFERENCES
- Standards for accreditation of medical education programs leading to the M.D. degree. Functions and standards of a medical school. II. Educational programs for the M.D. degree http://www.lcme.org/standard.htm#latestadditions. Liaison Committee on Medical Education, Washington, D.C. Updated 8 June 2004. Accessed 24 Feb. 2010.
- Geriatrics at Your Fingertips, www.geriatricsatyourfingertips.org; 2004-2005 web and PDA version; The American Geriatrics Society. Accessed 24 Feb. 2010.
- Epocrates: www.epocrates.com Rx & Medtools 2004-2005 version. Accessed 24 Feb. 2010.
- Geriatrics Review Syllabus: A Core Curriculum in Geriatric Medicine, 5th Edition by the American Geriatric Society.
- Swanson, A.G. and Anderson, M.B. Educating medical students. Assessing change in medical education – the road to implementation (ACME-TRI Report). Academic Medicine. 1993; 68(6 Supp.): Section 5, S35-S39.
- Moberg, T.F. and Whitcomb, M.E. Educational technology to facilitate medical students’ learning: background paper 2 of the medical school objectives project. Academic Medicine. 1999 Oct.; 74(10): 1146-1150.
- Andrews, P.U., Schwarz, J., and Helme, R.D. Students can learn medicine with computers: Evaluation of an interactive computer learning package in geriatric medicine. Medical Journal of Australia. 1992; 157:693-695.
- Kipp, D.E., Swagerty, D.C., Bonamino, G., and Paolo, A. Computer assisted instructional (CAI) modules in nutrition for medical students during the geriatric clerkship. Journal of the American Geriatric Society. 1998; 46:S23.
- Physicians’ use of handheld personal computing devices increases from 15% in 1999 to 26% in 2001.Harris Interactive 2001, Aug. 15.
- Waegemann, C.P. and Jessier, C. Documentation goes wireless: a look at mobile healthcare computing devices. Journal of the American Health Information Management Association. 2002 Sep.; 73(8): 36-39.
- Larkin, M. Can handheld computers improve the quality of care? Lancet 2001; 358:1438.
- Noonan, D. Wiring the new docs. Newsweek, 2002. Jun 24; 139 (25): 58-62.
- Wake Forest University. Palm, Inc. 2002.
- Helwig, A.L. and Flynn, C. Using palm-top computers to improve students’ evidence-based decision making. Academic Medicine. 1998; 73(5):603-604.
- Alderson, J.S. and Oswald, N.T. Clinical experience of medical students in primary care: use of an electronic log in monitoring experience and in guiding education in the Cambridge Community Based Clinical Course. Medical Education. (1999; 33 (6): 429-433.
- Criswell, D.F. and Parchman, M.L. Handheld computer use in U.S. family practice residency programs. Journal of the American Medical Intern Association. 2002; 9(1):80-86.
- Sumner, W. and Marshall, M. Family practice clerkship encounters documented with structured phrases on paper and hand-held computer logs. Proceedings American Medical Informatics Association Symp. 2000; (20 Suppl): 547-550.
- Adatia, F.A. and Bedard, P.L. “Palm reading”: 1. Handheld hardware and operating systems. Canadian Medical Association Journal. 2002 Oct. 1; 167(7): 775-780.
- Ellaway, R. and Masters, K. AMEE Guide 32: e-Learning in medical education Part 1: Learning, teaching and assessment. Medical Teacher. 2008 June 30; (5): 455-473.