ABSTRACT
From the authors’ experiences at a medical faculty where students are introduced to research early in their studies, members of the traditional pre-clinical medical science departments (Anatomy, Physiology, Biochemistry, Pharmacology and Medical Microbiology) have contributed significantly to the development of a research ethos amongst students, not only by supervising curriculum research, but also by providing extra-curricular research opportunities for students locally and abroad. Some of this work has resulted in scholarly achievements such as conference presentations and journal articles. Thus, medical scientists, through their supervision and mentorship of student research, have contributed to the preparation of young medical students for their clinical experience by developing skills that foster life-long learning. These important contributions should be duly acknowledged.
Abraham Flexner’s 19101 report changed the face of medical education across the globe. Flexner advocated that analytical reasoning and research (in his view, clinical) should be included in a physician’s training. Questions arising during patient care should serve as stimuli for inquiry and research to improve both teaching and patient care.1 Following this famous 1910 report, not only did research became an important part of the life of an academic, but the ‘traditional’ medical curriculum evolved to reflect the preclinical study of foundational medical sciences of Anatomy, Physiology, Biochemistry, Pathology, Pharmacology and Microbiology, followed by a period of clinical clerkships. Medical scientists were appointed (presumably on their research scholarship) to teach the “science” of medicine, while physicians took the responsibility of training students in the “art” of clinical diagnosis, treatment and management.
Although medical practitioners need to use evidence to inform their clinical decisions2, it is only relatively recently that the importance of student research opportunities in the medical curriculum has been appreciated. Even today, despite the paradigm shift in medical education to more integrated, student-centred and outcomes-based programmes, research opportunities for medical students vary from negligible3, through the inclusion of special study modules4 or perhaps extra-curricular summer research5, to the other extreme, where a research dissertation is required for graduation.6-9 The latter is the case for some German medical faculties and a handful of North American institutions that have adopted a scientific model of learning, involving the discovery of new knowledge. Perhaps the high priority given by medical educators and curriculum developers to designing a ‘core’ curriculum over the past few decades of curriculum reform has resulted in considerably less time being devoted to important issues such as research, ethics and social responsibility.
This situation is, however, changing. The increasing use of evidence-based medical practice in a cyberworld of readily accessible information requires a sound understanding of scientific methodology2, analytical and communication skills as well as an ability to critically appraise a vast literature.10-13 Research experience is therefore increasingly being recognized as integral to students’ understanding of medicine, and its integration into medical and health science curricula is now becoming widespread.3,13-18
Including student research in the medical curriculum has several positive spin-offs. In the first instance, patients should benefit from practitioners who critically use evidence to inform their clinical decisions.2 Improved practice and health care should enhance the reputation of the medical profession. Furthermore, in a profession plagued by declining numbers of academic physicians and “endangered” disciplines, research experience may influence career pathways, motivating some medical graduates to enter academic medicine or become involved in post-graduate research.14,16-19 Students too should benefit from their research experience. As they design research projects, generate hypotheses and analyze and interpret their data, they develop generic or transferable skills that prepare them for the challenges of their future careers in clinical medicine. 11-13,20 Research will also hopefully foster a life-long pursuit of knowledge, perhaps prompting post-graduate studies. It has been reported that research experience strengthens students’ residency applications, particularly in North America.3,9
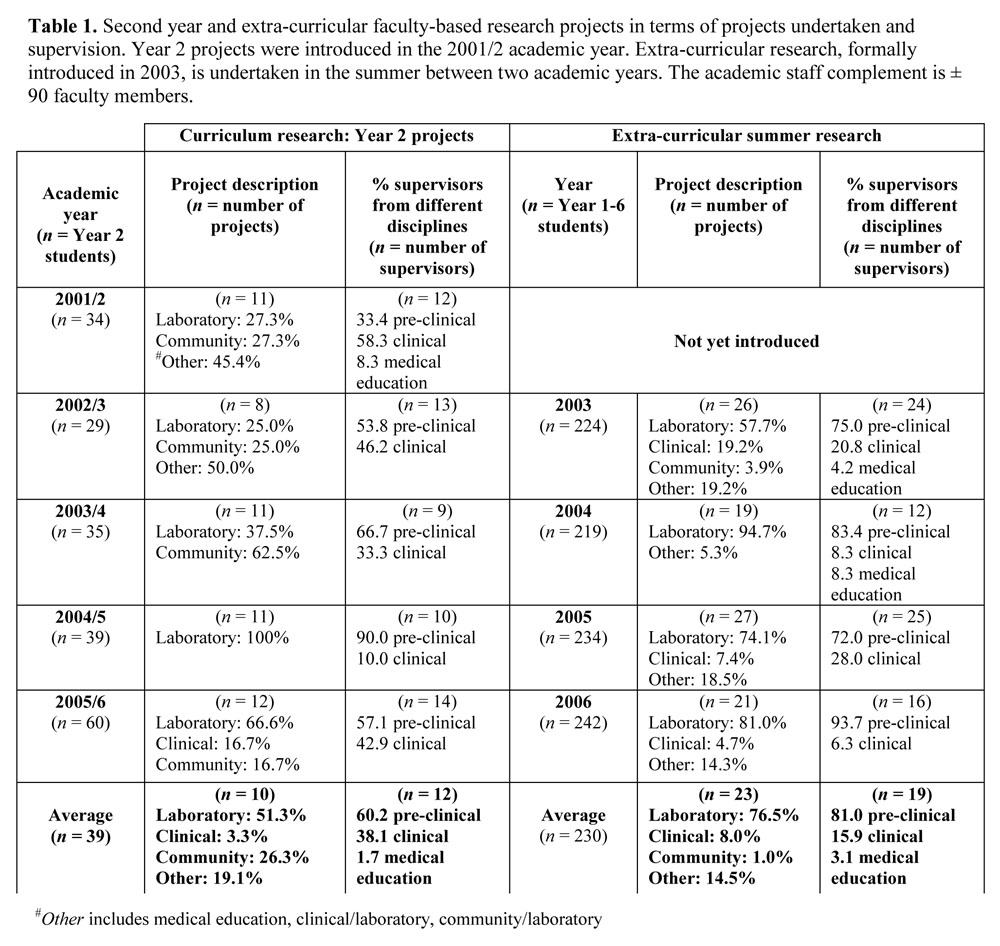
Recognizing the value of scientific and clinical research on the development of clinical reasoning skills and on the practice of evidence-based medicine, research projects were introduced in 2001 into the second year (Year 2 of Medical Sciences) of the undergraduate medical curriculum at the Faculty of Medicine and Health Sciences (FMHS) at the United Arab Emirates University (UAEU). The annual intake into the Faculty ranges from 29-60 students, while the staff complement is stable at around 90 members. Either individually or in groups of 2-5, students use protected time over a 4-5 month period for research. In addition, in 2003, extra-curricular summer research opportunities locally and abroad for students at any level of study were formally introduced. This extra-curricular research has become increasingly subscribed. The percentage of Year 1 students participating rose from 34.5% in 2003 to 58.5% in 2006. For the same period, participation amongst Year 2 students increased by 31.8% (from 11.8% to 43.6%). From humble beginnings, the Faculty’s undergraduate research programme (curricular and extra-curricular) has developed from strength to strength, the merit of which has been recognized by a recent external review committee – “Involvement of the medical students in research is impressive. Continuation of this programme is highly encouraged”.
As it had been approximately 5 years since the introduction of mandatory second year research projects and 3 years since summer research was first offered, an audit was called for (Table 1). Data collected from several sources (e.g. lists from the student project co-ordinator; year books; emails to faculty) took into account, amongst other things, types of projects offered and the disciplines of supervisors, as well as the scholarly outcomes (e.g. conference presentations, publications). In this discussion, we will utilize some of these data to support our view that medical scientists, through their supervision of undergraduate student research,
can foster a research ethos and promote a scholarship of discovery.
Immediately apparent from Table 1 should be the consistent contribution of medical scientists from the traditional pre-clinical disciplines of Anatomy, Physiology, Biochemistry, Medical Microbiology and Pharmacology to the supervision of both mainstream (51.3% of projects) and extra-curricular (76.5% of projects) research projects. Medical scientists accounted for 60.2% of Year 2 and 81.0% of the summer project supervisors, respectively. Projects have generally been laboratory-based, with many involving animal models to investigate human clinical conditions such as diabetes, cancer and neurological disorders. Apart from the supervisory contributions of members of Community Medicine, who supervise project work in the senior clerkship year, participation by clinical faculty has been erratic. This warrants exploration. A possible explanation may relate to their service responsibilities.
The importance of the medical sciences as the foundational underpinnings of the training and education of physicians cannot be disputed. As Finnerty (2004) pointed out, “the understanding of “basic sciences” is used everyday when a physician confronts a patient and attempts to generate a diagnosis and treatment plan”.21 By experiencing “science in action” during laboratory-based research, students witness first-hand the ramifications of a disruption of normal physiological and biochemical processes in the human body. Biomedical and scientific research thus has the potential to provide authentic and contextually relevant learning experiences for students. It is our view then that medical scientists in our Faculty have been able to incorporate such learning experiences into the undergraduate curriculum through their supervision of student research. According to Nancy Malkiel, a Dean at Princeton, “the research experience challenges and stretches students in ways that cannot be replicated even in the most rigorous and demanding coursework”.22
As medical scientist faculty members generally do not have clinical responsibilities, they can (as is the case in our faculty) contribute to the scholarship of an institution by promoting a research ethos amongst students. Many of our students have presented their research findings at international conferences (e.g. the Gulf Co-operation Council Medical Students’ and the Young European Scientists’ conferences), where some have won prizes. A number of students also appear as co-authors on peer-reviewed articles. This is the ultimate proof of scholarship.23 This is a win-win situation for everyone: students’ residency applications are strengthened, faculty promotion or tenure is potentially boosted through increased productivity and the prestige of the academy is enhanced.
In addition to promoting scholarship, medical scientists in our Faculty have also, by introducing young students to the rigors of scientific and biomedical research and reasoning, inculcated skills to equip students for their future studies and ultimately, their professional practice. To this end, students must independently (but under supervision) plan, organize, conduct experiments and subject their research findings to public scrutiny. Developing a project proposal, generating an ethics application, presenting it to the Ethics Committee, writing a progress report, creating a poster and finally, preparing a manuscript in the form of a journal article contribute not only to students’ communication skills but also to their information-handling, organizational, technical and numeracy skills. These have been identified as core skills for life-long learning.4 In addition, as students generally work in groups, they also learn to interact with colleagues, thereby potentially contributing to better management of learning in terms of giving and receiving feedback, accepting responsibility and, hopefully, reflecting on their contributions to the group.4 We have supporting evidence. During the past academic year, two second year students’ research project involved canvassing their senior colleagues’ perceptions of their research experience. When asked about the contribution of their research (curricular and extra-curricular) experience to the development of their generic skills (e.g. data analysis, information technology skills, time management, etc.), most students indicated a value in excess of 50%. Students from other institutions have also testified to the value of research on skills development, particularly critical thinking and analytical skills.10,13,20 In terms of the impact of research on their studies and future careers as medical doctors, research allowed one FMHS student to “understand diseases better”. He “also developed a sense of seriousness in my [his] life that made me [him] function better currently and hopefully in my [his] future studies”. For another student, research helped “bring up hypotheses for new research topics, especially topics in the clinical years”, while for a third, ”it helps understanding my [her] career and analyzing results before accepting them”.
It is our opinion that the medical scientists (and a handful of clinical researchers) at our institution have promoted in young students the ability to critically evaluate evidence, a practice that will inform their future clinical decisions. They will also have fostered skills that will enable students to be better communicators and team members. For some students, this research experience may motivate them to pursue a career in academic medicine, thereby potentially contributing to a new generation of urgently required clinician-researchers.17,18 As the first students exposed to curricular research are still in their early residency training, only time will tell whether they will become tomorrow’s clinical researchers. The research seed has, however, been sown.
Thus, at a time in medical education and health care when most clinicians spend a considerable proportion of their time attending to patients and supervising interns and residents, medical scientists have an important role to play in preparing young medical students for clinical practice through Boyer’s24 scholarships of discovery, application, integration and teaching. In integrated curricula, where early patient contact is advocated, research can contribute to the development of a number of skills that these young students will use in their studies and in clinical practice. Critical analysis, clinical reasoning and communication skills would be amongst these. In addition, providing research opportunities, including international exposure for those who have excelled (as happens at our institution), may potentially “career pipeline” some students into clinical disciplines in dire need of researchers.17 The valuable role of medical scientists in promoting a research ethos and scholarship in the institution through their supervision of student research should be duly acknowledged and rewarded.
REFERENCES
- Flexner, A. Medical education in the United States and Canada: A Report to the Carnegie Foundation for the Advancement of Teaching. New York: Carnegie Foundation, 1910.
- Sackett, D.L., Rosenberg. W.M.C., Gray, J.A.M., Hayes, R.B. and Richardson, W.S. Evidence based medicine: What it is and what it isn’t? British Medical Journal. 1996; 312: 71-2.
- Rhyne, R.L. A scholarly research requirement for medical students: the ultimate problem-based learning experience. Academic Medicine. 2000; 75: 523-524.
- Murdoch-Eaton, D.G., Ellershaw, J., Garden, A., Newble, D., Perry, M., Robinson, L., Smith, J., Stark, P., Whittle, S. Student-selected components in the undergraduate medical curriculum: a multi-institutional consensus on purpose. Medical Teacher. 2004; 26: 33-8.
- Schor, N.F., Troen, P., Kanter, S.L., Leving, A.S. The Scholarly Project Initiative: Introducing Scholarship in Medicine through a longitudinal, mentored curriculum programme. Academic Medicine. 2005; 80: 824-31.
- Altunbas, A., Cursiefen, C. Research activities of medical students in Germany using as an example the Wurzburg University Clinic. Deutschse Mediese Wochenschrift. 1998; 15: 617-20.
- Cursiefen, C., Altunbas, A. Contribution of medical student research to the MedlineTM-indexed publication of a German medical faculty. Medical Education. 1998; 32: 439.
- Dewey, M. Students’ evaluation of research during medical studies: Medical dissertation in Germany. Medical Education. 2003; 37: 278-80.
- Chongsiriwatana, K.M., Phelan, S.T., Skipper, B.J., Rhyne, R.L., Rayburn, W.F. Required research by medical students and their choice of a women’s health care residency. American Journal of Obstetrics and Gynaecology. 2005; 192: 1478-80.
- Frishman, W.H. Student research projects and theses: should they be a requirement for medical school graduation? Heart Disease. 2001; 3: 140-4.
- Whittle, S., Murdoch-Eaton, D.G. Development of lifelong learning and self-evaluation skills through special study modules. Medical Education. 2001; 35: 1066-90.
- Whittle, S.R., Murdoch-Eaton, D.G. Student-selected projects: Can they enhance lifelong learning? Medical Teacher. 2002; 24: 41-4.
- Joubert, G. Research by pre-clinical undergraduate medical students. Medical Education. 2006; 40: 459-89.
- Friedrich, M.J. A novel programme seeks to take clinical scientists off the endangered species list. Journal of the American Medical Association. 2003; 290: 1019-20.
- Zier, K., Stagnaro-Green, A. A multifaceted programme to encourage medical students’ research. Academic Medicine. 2001; 76: 743-7.
- Solomon, S.S., Tom, S.C., Pichert, J., Wasserman, D., Powers, A.C. Impact of medical student research in the development of physician-scientists. Journal of Investigative Medicine. 2002; 51; 149-56.
- Halpain, M.C, Jeste, D.V., Trinidad, G.I, Wetherell, J.L., Lebowitz, B.D. Intensive short-term research training for undergraduate, graduate, and medical students: early experience with a new national-level approach to geriatric mental health. Academic Psychiatry. 2005; 29: 1. http://ap.psychiatryonline.org. Accessed 7/22/2006.
- Wagner, R.F., Ioffe, B. Medical student dermatology research in the United States. Dermatology Online Journal. 2005; 11: 8. http://dermatology.cdlib.org/111.commentary/msresearch/wagner.html, Accessed 7/22/2006.
- Segal, S., Lloyd, T., Houts, P.S., Stillman, P.L., Jungas, R.L., Greer, R.B. The association between students’ research involvement in medical school and their postgraduate medical activities. Academic Medicine. 1990; 65: 530-3.
- Jacobs, C.D., Cross, P.C. The value of medical student research: The experience at Stanford University School of Medicine. Medical Education. 1995; 29: 342-6.
- Finnerty, E.P. Why the basic sciences? Journal of the International Association of Medical Science Educators. 2004; 12(1). http://www.iamse.org/artman/publish/article_170.shtml. Accessed 8/24/2007.
- Malkiel, N.W. (unknown). Spotlight: undergraduate research, scholarship, and creative activity. http://www.reinventioncenter.miami.edu/Research%20spotlight.html. Accessed 9/3/2007.
- McLean, M., Howarth, F.C. Does undergraduate student research constitute scholarship? Drawing on the experiences of one medical faculty. The Journal of Scholarship of Teaching & Learning. In press.
- Boyer EL. Scholarship Reconsidered: Priorities of the Professoriate. San Francisco: Jossey-Bass, 1990.