ABSTRACT
Medical curricula have traditionally focused on content delivery with students as onlookers, primarily with a didactic lecture format. Even group teaching methods require faculty development of the structure, objectives, and much of the content delivered in the group setting, without a formal and sustained student presentation format. There is minimal reliance upon student-generated curriculum delivery. Both methods and contact hours to support student acquisition of competencies in medical education that drive research, data analysis, composition and presentation skills are needed in a curriculum, particularly within basic science disciplines. This report describes a method that supports multiple skills-based competencies as well as delivery of curricular knowledge-based content with the use of student presentations in the form of clinical-pathologic correlation (CPC) exercises by students to peers. Deployment of these CPCs with a rising class size occurred over a period of 6 years in a medical school pathology course. Course ratings remained high during that time, and student success in the course was supported with these CPCs.
INTRODUCTION
Medical teaching has evolved to include curricular components that support achievement of competencies in the domains of knowledge, skills, and attitudes.1 Traditionally, curricula have been biased toward components such as lectures that support the knowledge domain, with standardized multiple choice question examinations to test the acquisition, retention, and use of knowledge.2 Meaningful instruction with assessment involving skills and attitudes has been harder to achieve, particularly within basic sciences, though some models do exist.3 The preclinical basic sciences typically devote a majority of their assigned curricular time to a lecture format, according to the Association of American Medical Colleges (AAMC) Curriculum Management and Information Tool (CurrMIT).4
Students with different learning styles may benefit if multiple learning methods are applied.5 A subset of curricular time can be deployed through group teaching methodologies such as case-based, team-based or problem-based learning. However, within those group processes students are not typically made individually accountable for specific skills competencies such as communication, informatics, data analysis, critical thinking, and translational research. Faculty are typically responsible for developing group exercises, and the students then work within the resulting structured framework to primarily acquire knowledge content. In the current study a plan was devised by the author that addresses multiple skills-based competencies outlined in the LCME standards of accreditation (ED-1-A, ED-12, ED-17, ED-19, and ED-28), the AAMC Medical School Objectives Project (MSOP) medical informatics competencies, replaces faculty lectures, and allows students responsibility for development and presentation of CPC exercises containing knowledge content.6,7
METHODS
The Systemic Pathology course ran for 22 weeks in the 2nd year of the curriculum at the Florida State University College of Medicine from 2002 to 2008, encompassing 6 medical student classes, with the author as course director. Each class was assigned to groups of 3 to 4 students for each clinical-pathologic correlation (CPC) exercise. The total number of CPC groups ranged from 10 for the initial class size of 30 students to 26 groups for a class size of 102 in the 2007-8 academic year. When the class size exceeded 50 students in the 2005-6 academic year, the class was divided in half (cohorts A and B) and two separate CPCs given, one for each half of the class, sharing the time with two other curricular exercises (Table 1).
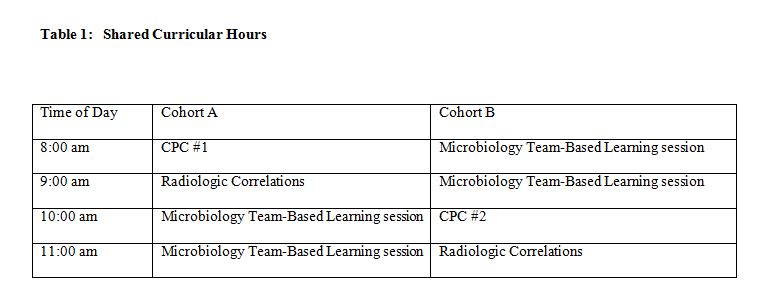
Cohorts A and B attended separate classrooms, with one or more faculty per classroom. The faculty stayed in one room and the cohorts switched rooms at 10:00 a.m. Thus, the faculty repeated facilitation of each exercise for each half of the class, but the students did not repeat sessions. A total of 10% of course instructional hours were devoted to CPCs, with the number of lecture hours reduced to provide adequate time.
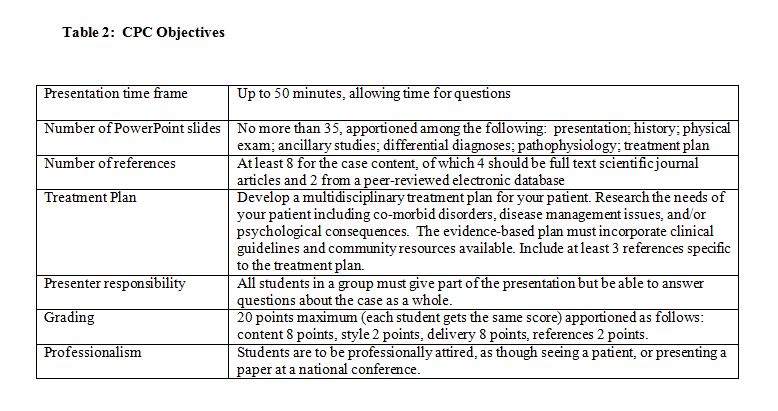
The students were given a detailed guide for constructing their CPC presentation. The CPC topics were assigned by the course director and were chosen to integrate with the course content delivered concurrently. The topics were not covered elsewhere in the course, so the knowledge-based content of CPCs was delivered solely by students. The topics included disease entities such as androgen insensitivity syndrome, paroxysmal nocturnal hemoglobinuria and angiodysplasia that were uncommon but had mechanisms of disease that were part of the course learning objectives. The topics chosen were not covered in detail in the course textbook (Robbins & Cotran Pathologic Basis of Disease, Elsevier-Saunders, Philadelphia, PA, ISBN: 978-1-4160-3121-5), and they required research with literature review by the students, along with data analysis. The students were directed to be creative in developing their own presentation history for a single patient. The CPCs were delivered as PowerPoint-based presentations in the classroom using the general objectives outlined in Table 2.
The CPC was presented by students in a reverse format: instead of an expert starting with an unknown case with data to analyze and deciding on a diagnosis in a presentation before an audience that only listens, the student presenters were given the diagnosis and developed the case to present as an unknown to their peers. Their classmates had to respond to the progressive disclosure of the data by interacting and developing a differential diagnosis list and suggesting ways to work up the patient before moving on to the next PowerPoint slide. The student presenters were encouraged to direct questions about the case to their peers so as to facilitate interaction. The students were advised that the journey was as important as the destination for this exercise. About halfway through the CPC, the presenters compared their differential diagnosis list to that developed by their classmates, and then the diagnosis for the case was revealed. The presenters then finished with a detailed discussion of the pathophysiology of the disease and their treatment plan.
All students in the class were responsible for reviewing the PowerPoint files posted following each presentation to the course electronic website (Blackboard®). At least one examination question was formulated by the course director from each PowerPoint file. All presenting group members were required to collaborate and participate in development of both content and presentation. Limiting groups to no more than 4 students facilitated sharing of tasks within the 50 minute time frame of the presentation. The grade for the CPC was assigned by the author, who attended all presentations and provided informal feedback.
RESULTS
The CPC contributed 3% of the total assessments factored into the grade for the course. Students were told at the beginning of the course that it was expected every group would attain the maximum score. Of the 349 students enrolled over 6 years, 85% received the maximum score, 14% received a deduction of 1 point because the group documented fewer references than required, and 1 group (1 %) received a 2 point deduction for inaccurate data. The overall course performance was enhanced for all students via the CPC exercise and no student grade diminished because of the CPC. When the class was divided, half attending the one presentation and reviewing only the PowerPoint slides of the second presentation, there was no statistical difference in performance between cohorts A and B on presentation-derived examination items.
Group members reported spending a minimum of 1 hour and maximum of 4 hours individually developing the content for the presentation. Collectively, group members spent an average 2 hours putting the presentation together. Groups averaged 1 hour meeting with the course director for mentoring regarding the process and content.
The average Systemic Pathology course rating, using a Likert scale, was 4.63 (out of 5 possible) for the 6 years in which the CPC exercise was part of the course. The CPC was not a specific evaluation item. No written comments specific to CPCs were made by any students on course evaluations.
DISCUSSION
This CPC exercise illustrates how preclinical medical students can deliver assessed course content as part of their curriculum, rather than faculty, and do an equal or better job when given explicit instructions. These students in a second year pathology course were not complete novices at PowerPoint presentations. They had given presentations (as part of small groups of 4 to 6 students) in first year anatomy and cellular biology/histology courses, and in a second year microbiology course, but those prior presentations averaged only 10 to 15 minutes in length. Thus, students could build upon prior experiences through curricular vertical integration. Students want to impress their peers, so the quality of the presentations was equivalent to faculty lectures. Every CPC presentation developed by the students was unique and exhibited creativity.
Informatics skills were reinforced as part of the AAMC’s MSOP concerning medical informatics competencies.7 Students used the library’s electronic resources to perform their research of the medical literature and then organize their data. Data analysis and critical thinking were required because the presentation could not be developed from a sole information source, and the disease processes assigned as topics were uncommon, complex and the focus of ongoing research. A treatment plan had to be formulated to fit the data. A shared project to produce a poster or paper to reinforce such skills has been described.8 However, this CPC format required a PowerPoint presentation that further enhanced informatics skills with application of direct peer-to-peer communication.
The skills-based competencies of communication, data analysis, critical thinking and research applied to patient care are typically not incorporated into basic science teaching and assessment, but left to the clinical skills components of the curriculum.9 Those skills were assessed via the CPC through the presentation format, based upon the successful completion of the task assigned as well as quality of the presentation. Regardless of the scores on knowledge-based assessments in the course, all students performed admirably for this exercise. It could be argued that a high score was a “given” for this CPC exercise and served no discriminatory function, but on a criterion basis, the students did what they were asked to do, met the objectives, and demonstrated competence.
Incorporation of communication skills practice and assessment into the curriculum is difficult to achieve but has shown benefit for medical student functioning in the clerkship setting.10,11 Assessment of communication skills is often incorporated into an objective structured clinical examination (OSCE). However, each OSCE station does not typically require sustained and formally organized presentations and occurs in a one-on-one setting. The exercise described here reinforced communication skills because each group of students had to work together to produce a single presentation, then give a seamless presentation to their classmates over a sustained time frame (50 minutes). The use of a 10 to 15 minute “mini-lecture” by student groups has been described, but not longer presentations such as the CPC format.12 Student presentations have been utilized to facilitate their future teaching role as residents.13
The structure and objectives of this CPC exercise were designed to keep students focused and prevent them from spending too much time on the exercise. The students were advised that quality content for knowledge yield was more important than computer wizardry that could become a time sink in preparation of the presentation. The 3% contribution of the CPC to the overall course grade was pegged at a level deemed high enough to make the effort worthwhile to students while low enough so as not to mask poor performance on standard knowledge-based examinations. Given the lack of specific comments by the students regarding the CPCs, this formula appears to have worked.
This exercise included novel approaches to scheduling curricular events. First, the contact hours were shared among curricular components, keeping the contact hours constant for students, while increasing the contact time required for faculty. Smaller cohorts of students afforded more opportunities for classroom interaction. Though faculty time required in attendance for this format was effectively doubled, preparation time was not. Second, a significant portion (10%) of instructional hours was given to students for meeting competencies while delivering knowledge content, making the student CPC exercise an alternative to lecture hours.
The possibility of being asked questions motivated the student presenters to be thorough in their preparation, understanding of the topic and collaboration. The audience initially were reluctant to ask questions of their presenting peers, but were encouraged to participate by pointing out that the presenters had made the effort to gain expertise and that they should be honored with the opportunity to share their knowledge. The students also learned that an “I don’t know” response could be followed up with additional research and an answer e-mailed to the class following the presentation.
In mentoring the students, it became apparent that they gained insight into the scientific process of investigation. Whereas textbooks present what appears to preclinical medical students to be solid factual uncompromising information, the medical literature is not so straightforward. Students had to apply data analysis and critical thinking to synthesize their research on a topic into a cogent presentation. They often had to present multiple viewpoints or reconcile conflicting information.
In retrospect, LCME standard ED-32 (narrative descriptions of student performance and of non-cognitive achievement) could have been included as part of the assessment strategy for this exercise. Informal comments were made to the students during mentoring and following the presentation, but such comments were not part of a written record. There were no incidents involving professional behavior during the presentations that required action be taken.
Though no formal attendance role was taken during these exercises, there were three factors driving attendance: a graded quiz in concurrent Microbiology team-based learning sessions, questions directed to students in any of these sessions, and a small cohort size. Students missing from these curricular exercises had to obtain formal excused absences, according to standard school policy.
CONCLUSION
The CPC exercises afforded students an opportunity to apply communication, informatics, research and critical thinking skills in a preclinical basic science course. Knowledge-based content was delivered by students to peers in lieu of faculty lectures. All students demonstrated competency in fulfilling objectives outlined for the CPC.
REFERENCES
- Litzelman D.K., Cottingham A.H. The new formal competency-based curriculum and informal curriculum at Indiana University School of Medicine: overview and five-year analysis. Academic Medicine. 2007;82:410-21.
- Kassebaum D.G., Eaglen R.H. Shortcomings in the evaluation of students’ clinical skills and behaviors in medical school. Academic Medicine. 1999;74:842-9.
- Derstine P.L. Implementing goals for non-cognitive outcomes within a basic science course. Academic Medicine. 2002;77:931-2.
- Association of American Medical Colleges. CurrMIT (Curriculum Management & Information Tool): http://www.aamc.org/meded/curric/start.htm [Accessed July 24, 2009].
- Van der Veken J., Valcke M., Muijtjens A., De Maeseneer J., Derese A. The potential of the inventory of learning styles to study students’ learning patterns in three types of medical curricula. Medical Teacher. 2008;30:863-9.
- Liason Committee on Medical Education. Current LCME Accreditation Standards. Functions and Structure of a Medical School: Standards for Accreditation of Medical Education Programs Leading to the M.D. Degree, June 2008: http://www.lcme.org/functions2008jun.pdf [Accessed July 27, 2009].
- McGowan J.J., Passiment M, Hoffman HM. Educating medical students as competent users of health information technologies: the MSOP data. Studies in Health Technology and Informatics. 2007;129(Pt 2):1414-8.
- Krilowicz B.L., Downs T. Use of course-embedded projects for program assessment. American Journal of Physiology. 1999 Jun;276(6 Pt 2):S39-54.
- Wagner P.J., Lentz L, Heslop SD. Teaching communication skills: a skills-based approach. Academic Medicine. 2002;77:1164.
- Headly A. Communication skills: a call for teaching to the test. The American Journal of Medicine. 2007;120:912-5.
- Yedidia M.J., Gillespie C.C., Kachur E., Schwartz M.D., Ockene J., Chepaitis A.E, Snyder CW, Lazare A, Lipkin M Jr. Effect of communications training on medical student performance. Journal of the American Medical Association. 2003;290:1157-65.
- Love R.R. Methods for increasing active medical student participation in their own learning: experience with a single 30-hour course for 111 preclinical students. Journal of Cancer Education. 1990;5:33-6.
- Pasquale S.J., Pugnaire M.P. Preparing medical students to teach. Academic Medicine. 2002;77:1175-6.