ABSTRACT
The first-year medical curriculum at The University of Texas Medical School at Houston (UTMSH) comprises traditional discipline-based basic science courses and an Introduction to Clinical Medicine (ICM) course in which students learn the rudiments of the patient interview and physical exam. Integration of material across diverse courses is a key aspect of modern, competency-based curricula, and can be difficult to achieve in a traditional, discipline-based curriculum. To accomplish a degree of integration, the first-year course directors developed Clinical Applications, a course that meshes information presented in the basic sciences with skills learned in the Introduction to Clinical Medicine course using a team-based learning approach.
Seven integrative problem-solving sessions were introduced into the first year curriculum, four in the first semester and three in the second. These sessions utilized clinical scenarios of patient problems, and integrated content from at least three first-year courses in each session. A concerted effort was made to incorporate concepts from first-semester courses into sessions in the second semester, thereby promoting vertical and horizontal integration. Clinical scenarios were diverse and included topics of infertility, premature birth, sickle cell anemia, HIV infection, diabetes mellitus, renal failure, cardiovascular disease, cancer, neuronal pathways and pain, and travel medicine.
Results from the inaugural year of this course suggested that clinical problem-solving exercises presented in a team-based learning format were effective for integrating basic science concepts in a traditional discipline-based curriculum. The course also facilitated communication among all the directors of first-year courses and encouraged more integration in the first-year curriculum.
INTRODUCTION
In recent years, the majority of medical educators have come to accept that “there needs to be a better integration between clinical experiences and the basic science courses.”1 Although rote learning is useful and advantageous in certain learning situations,2 it has become evident that simple regurgitation of facts does not make a good physician and implant medical competence into students.1 There have been enormous changes in mechanisms of health care delivery and an explosion in technology, medical developments and medical research, resulting in students facing massive amounts of new information to integrate and study. It was therefore inevitable that educational trends had to address not only what medical students learned, but how they learned.3,4
With the inevitable changes to curriculum, aims, scope and outcomes, and new teaching models, it is paramount that beneficial transformations are made to medical school teaching strategies. New strategies, such as those found at CanMEDS,5,6 the University of Dundee Centre for Medical Education (http://www.dundee.ac.uk/meded/frames/home.html) and the teaching academy at the College of Physicians and Surgeons at Columbia University (http://www.education.cumc.columbia.edu/glenda_garvey/recipients.html), are becoming standard methodologies to facilitate teaching and facilitation is critical in light of the heavy burden on today’s medical student, brought about by the increase in information available in an ever changing electronic world.
The overall objective of the UTMSH Medical School curriculum is that students acquire the knowledge, skills, behaviors and attitudes that will lead to their becoming competent and compassionate physicians. The list of core competencies states that graduating students will “understand and have knowledge of the scientific principles including genetic, molecular, and physiological mechanisms basic to the practice of clinical medicine, and be able to use these principles in providing health care of common diseases.”7 Cognizant of the academic culture of our medical school, we have had to re-evaluate what components were needed in our curriculum in order to produce not only the type of student physician that we, as instructors, wanted, but more importantly, the type of physician that patients would desire.8 This type of student physician is a person who 1) communicates well, 2) can define a problem, 3) knows treatment options, 4) shows respect for the patient and others, 5) works well in a team, and 6) accepts constructive input and can self-reflect accordingly.9
One area that most faculty thought could be developed was the ability of first-year medical students to apply principles presented in their basic science courses (Biochemistry, Developmental Anatomy, Gross Anatomy, Histology, Immunology, Microbiology, Neuroscience, and Physiology) and skills learned in Introduction to Clinical Medicine (ICM) into formulating solutions of clinically related problems. In order to help them develop this competency, the first-year course directors strived for a method of teaching that was interactive, integrative, and enjoyable for the students; a course that drove the students to think individually and as a team, while giving them an understanding of the value of competency in the basic sciences. We chose team-based learning (TBL), which had been applied in a few of our first-year courses, as the teaching modality to best satisfy these requirements.
Team-based learning (TBL) is a tried and trusted teaching method that, when utilized properly, is a valued addition to the medical school curriculum.10 TBL consists of three learning phases: 1) the preparation phase in which students prepare for the TBL sessions by completing assigned reading, 2) the readiness assurance process during which students take a short test on the assigned reading, first as an individual and then as a team, 3) and the application phase, in which the concepts the students have learned in the first two phases are applied to solving problems.11 This strategy has the advantage that it can be utilized in classrooms with high student-to-facilitator ratios.12,13 TBL has been introduced into many facets of medical and health science education, from the undergraduate stage14 through the clerkship level,15 since with this approach, active learning is fostered, and student attitudes and interactions are improved.13 Indeed, a recently published book details how to use TBL advantageously in health professions education, again stressing the positives of active participation, better knowledge retention and the promotion of self-directed learning.16 Essential to successful implementation is that all participants, from administrators to faculty, invest sufficient time and resources to develop TBL exercises to ensure desired, positive outcomes.17
In this report, we describe the construction and implementation of an integrative course at our institution entitled Clinical Applications. We used an innovative implementation of TBL as the teaching modality to help first-year medical students integrate principles learned in their basic science courses and skills learned in ICM, by applying these principles and skills to the solution of problems presented in clinical scenarios. Overall, Clinical Applications was well received by students,18 but with a few surprising outcomes that may impact the future administration of the course. This is a course that we believe will strengthen students’ skill sets as they journey towards becoming knowledgeable, competent physicians.19
METHODS
Students were asked to complete team-based learning tasks within a 90-minute session; seven such Clinical Applications classes were held throughout the first year, with two distinct cases revolving around a central theme presented in each session. The first-year class was divided into 40 teams of six students, corresponding to their Gross Anatomy tank groups, thereby increasing both the continuity and cohesiveness of learning within each team. Students prepared for the integrative sessions by individually completing pre-assigned readings and reviews of targeted basic science lecture material. Mastery of this material was assessed by a readiness assurance quiz. Students first take the quiz individually (IRAT – Individual Readiness Assurance Test), and then retake the quiz as a team, arriving at an answer by team consensus (GRAT – Group Readiness Assurance Test).20 User-friendly ‘scratch off’ answer sheets were employed for the GRAT to provide immediate feedback of success in answering the question (Immediate Feedback Assessment Technique [IF*AT], Epstein Educational Enterprises, Princeton Junction, NJ, USA). The groups were then given a clinical scenario that formed a framework for a series of related problem sets to be solved through group discussions, followed by feedback from faculty presenters. Teams composed a one-page written justification of their answer to each designated problem within the set and submitted the justification for grading.
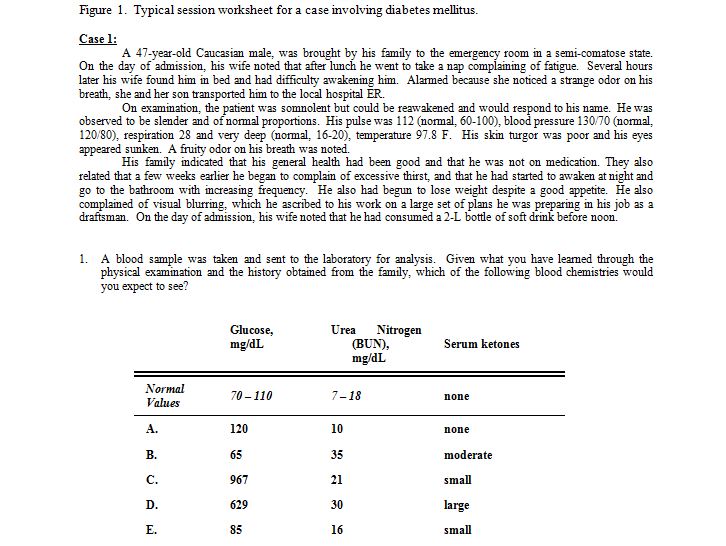
Following intra-group discussions, team presentations of answers were facilitated by the first-year course directors, a process best accomplished when all first-year course directors were present to reinforce horizontal and vertical integration. An example of a session worksheet, this one pertaining to the biochemistry/chemistry of diabetes, is shown in Figure 1.
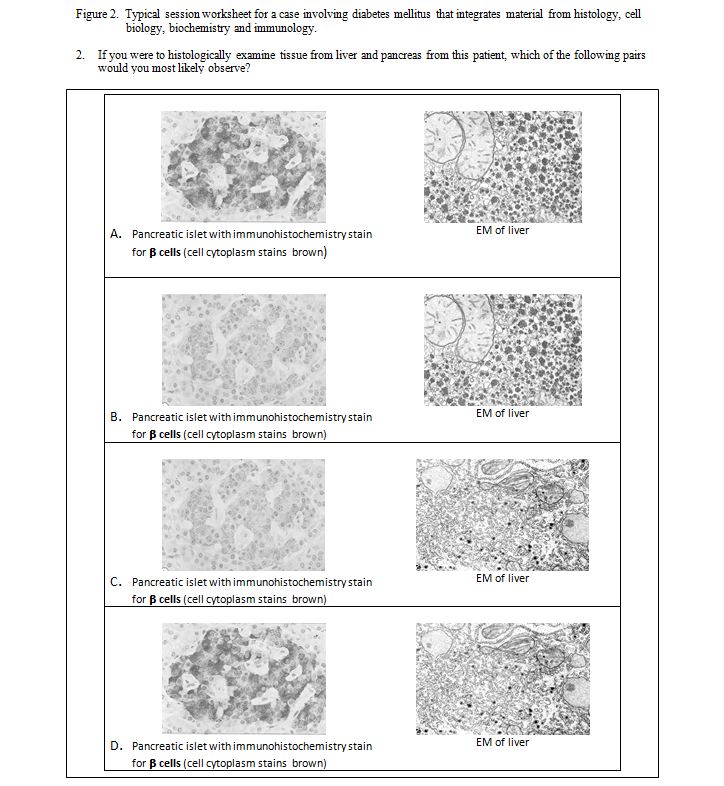
As different aspects of the clinical scenario were explored, concepts relating to diverse first year course instruction were introduced. Figure 2 shows a question from the same diabetes case, illustrating how elements of histology, cell biology, biochemistry and immunology were combined to synergistically develop a diagnosis. In this question, students were shown immunohistochemical staining of pancreatic acinar cells and transmission electron microscopy of liver structures, and asked to identify the pair of images demonstrating corresponding changes associated with uncontrolled Type I diabetes.
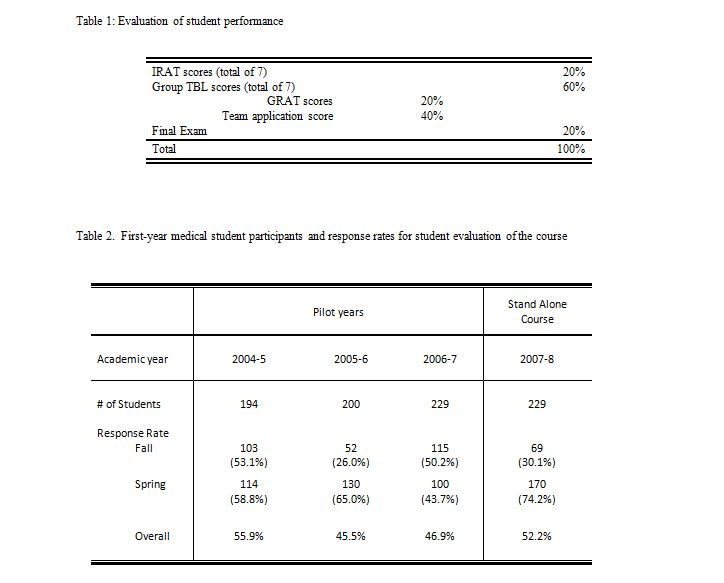
Students were evaluated based on i) their individual performance on the IRATs; ii) on their team’s performance on the GRATs and team written justifications, and iii) on their performance on a team-task based final exam (Table 1). Online evaluations by the students of the course content and structure were administered at the end of each semester.
Prior to implementing Clinical Applications as a stand-alone course, the course was piloted for three years beginning in 2004. The course was conducted under the administration of ICM, the only year-long course in the first-year curriculum at that time. During the first two years of this pilot stage, a modified version of team-based learning was introduced that used only the application phase of the process. In the last year of piloting the process, the complete TBL strategy was utilized, as described above. During the three-year pilot phase, clinical scenarios were presented in a sequential fashion to the whole class using PowerPoint® slide presentations with application exercises introduced at appropriate intervals.
Once Clinical Applications became a stand-alone course, the clinical cases and application exercises were distributed to the teams as a packet of printed materials. This encouraged the students to work at a faster pace, thereby helping the faculty complete the sessions in the allotted time. The final exam was given in a format similar to a Clinical Applications session in that clinical scenarios were presented and questions were asked about the problems presented within that case. Students were to synthesize their answers using the knowledge they had gained from their basic science and ICM courses. The answers to these questions were short answer or brief essays that were compiled by team consensus. The teams submitted their answers electronically using the Digital Dropbox on the course Blackboard® site within the allotted time. All team members received the same final exam score.
To measure their perceptions of the integrative sessions, students were given the opportunity to evaluate the course after each semester using the survey tool of Blackboard®. Survey content and items were generated to assess whether students thought the sessions helped them understand material presented in the ICM course and their basic science courses and whether the sessions helped them apply basic science concepts to clinical situations. Other items queried whether the students perceived themselves and their team members as being actively engaged in the sessions, their perceptions and conclusions as to the usefulness of the readiness assurance process, the effectiveness of using hardcopy printouts of the cases and problems, and the format of the final exam. Student responses for these items were on a five-point Likert scale. Students’ opinions about the size of the teams and the number of TBL integrative sessions that should be presented over the course of the year were solicited. In addition, students were given the opportunity to submit written comments about 1) how they thought student participation could be increased, 2) the format of the final exam, and 3) how the course might be more effective.
A focus group of 11 students recruited by the student evaluation committee was convened and facilitated by the Office of Educational Programs after the first year of Clinical Applications as a stand-alone course. The purpose of the focus group was to gather additional input from students regarding strengths and weaknesses of the course, administration of the course, course improvement, and whether the course helped them apply basic science principles to clinical problems. All comments were recorded anonymously and compiled by the Office of Educational Programs before being forwarded to the faculty of Clinical Applications for their careful review.
RESULTS
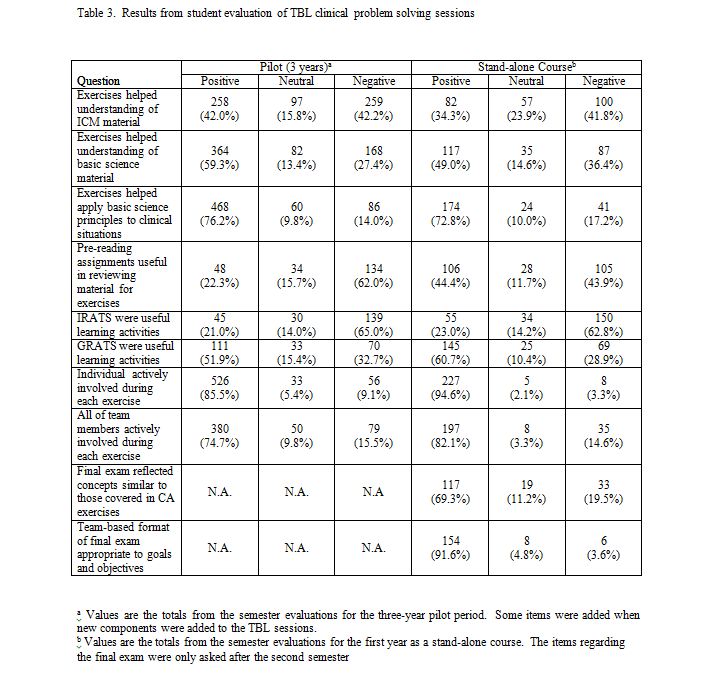
The number of students that participated in the course during the three pilot years and the first year as a stand-alone course, as well as the response rates on the online student evaluation surveys, are presented in Table 2. The increase in the number of participants is a result of a decision by UTMSH to increase the class size by 15%. Since the evaluations were voluntary and administered on-line, the response rates are variable. Increased response rates were obtained when students received several email reminders.
The feedback received from the online student surveys is presented in Table 3. The five-point Likert scale has been simplified to Positive, Neutral and Negative responses. The combined feedback for the first three years of the pilot course is compared with that for the first year of Clinical Applications as a stand-alone course. The total number of responses varied for each question because not all students responded to all of the items in the survey. As can be seen from Table 3, the feedback received during the first year of the stand-alone course is consistent with that obtained during the three pilot years, and our comments will focus on the stand-alone course, unless otherwise noted. A sizable majority of students (72.8%) responded that the Clinical Applications sessions help them to better apply their basic science knowledge to clinical manifestations of disease, and augment their understanding of how basic science concepts are useful in comprehending disease initiation, diagnosis and progression. Fewer students (49.0%) agreed that the sessions were useful in helping them understand the actual material presented in their basic science courses, and that the exercises helped them understand concepts in ICM (34.3%). The proportion of students who felt that the pre-reading assignments were useful in preparing for the exercises in the stand-alone course (44.4%) increased from that of the pilot years (22.3%). While most of the students responded that the GRAT was a useful learning activity (60.7%), the opposite was true with their views regarding IRAT exercises (23.0%).
A large majority of the students felt from the inception of the integrative TBL sessions during the pilot years that they and their team members were actively engaged during each of the exercises (85.5% and 74.7%, respectively). However, when the case scenarios and application exercises were distributed as printed paper handout packets (stand-alone course), instead of via projected PowerPoint® images (pilot years), students’ perception of their own and their team members’ active participation increased (94.6% and 82.1%, respectively). In addition, since beginning these TBL sessions 79.6% of the respondents (682) believed that the size of the team (5-7 members) is appropriate and 82.7% (707) responded that the number of sessions per year should increase or stay the same (data not included in Table 3).
Following the introduction of a team-based final exam with the stand-alone course, students indicated in their evaluations that they enjoyed the format of the exam; 69.3% responded positively when asked if the final exam reflected concepts covered in the Clinical Applications sessions and 91.6% indicated that the team-based format was appropriate for the goals and objectives of the course. Written comments indicated that although the exam was challenging, students appreciated being able to utilize a group format to discuss the clinical problems and formulate a team response. Comments included: “The final exam was an excellent way to end the class. It was based on team work and figuring out medical cases with the help of peers.” and “The final exam was actually an enjoyable experience because teams were left on their own to solve cases using available resources.” The focus group presented similar conclusions to those of the on-line evaluation, while also highlighting ways to improve the administration of the course. For example, one suggestion was to use the format of the final exam for all of the sessions.
DISCUSSION
Results from the inaugural year of the Clinical Applications course suggest that clinical problem-solving exercises presented in a TBL format are an effective method for both integrating basic science concepts taught in a traditional discipline-based curriculum and for the synthesis of information in solving patient-related problems. Overall, the format of the course easily accommodates a large number of students while supporting a congenial small group atmosphere with willing faculty as facilitators21 giving the students a patient-centered, case-based, early learning opportunity.22 The format fosters and emphasizes student-student interactions and active student participation, with appropriate faculty-student interaction during which clinical faculty often relate personal experiences in dealing with clinical cases similar to those being discussed. In retrospect, the course provided a “relaxed” atmosphere, often allowing for humorous aspects of cases to complement the serious nature of clinical presentation and therapeutic interventions. The end result was to reinforce basic science concepts, providing a novel mechanism to attain teaching objectives.
Results from the student surveys suggest that the primary goal of developing the ability of first-year medical students to apply basic science principles to the solution of clinically related problems was successful. That fewer students thought the sessions were useful in helping them understand the concepts presented in the basic science courses and in their ICM class is not totally unexpected owing to the nature of the TBL method. Team-based learning sessions are designed to enable students to apply previously learned concepts and skills by solving problems related to those concepts and skills.23 Primary comprehension of the informational content comes through individual study of the material presented in the didactic and skills sessions. Despite the results of the student evaluation, we would argue that if the exercises helped students apply basic science principles in solving clinical problems, they also helped the students to gain an increased understanding of those principles.
An interesting observation is the discrepancy in the student perceptions of the usefulness of the IRAT and GRAT as learning activities. It suggests that the students perceive the IRAT as purely summative in nature, whereas, through team discussion and construction of a consensual answer, the GRAT helps them to correct misconceptions and increase their comprehension of the material being tested. Since the average GRAT score is universally higher than the average IRAT score (data not shown), it appears that many students do indeed learn from team discussions of the quiz items.
A somewhat surprising outcome (from data in Table 3, written comments and focus group responses) was the number of students that perceived pre-reading as an “extra” or “superfluous” task that would be better received as part of the actual lesson. This may reflect the heavily weighted didactic lecture-based format of the first-year curriculum at UTMSH, as well as the inexperience by students of this teaching modality. It is possible that students may wait to read assigned texts or syllabi until after a lecture is given in an attempt to review material and integrate this with their lecture notes. Another surprising outcome was the relative success of traditional, compared to modern, educational methods and technologies. PowerPoint® presentations were initially used as the primary tool in presenting the case scenarios and group application exercises, and we tried using an audience response system for simultaneous reporting of answers by all the teams. We discovered however, that hardcopy paper case scenarios and application exercises led to better sessions, better student-student and student-faculty interactions and exchanges, and better resolution of disagreements among students. The change in format to the paper cases facilitated a more collaborative atmosphere allowing for a better overall experience for both the overloaded students and the time-constrained faculty. PowerPoint® presentations are still used, albeit as an adjunct learning tool, to help in the clarification of particular teaching points. The return to the use of response cards for teams to report their answers eliminated technical difficulties that occasionally arose with the audience response system and the tendency for students to “play” with the clickers or race to be the first to respond rather than fully discussing the problem.
This integrative, team-based learning course helps satisfy our goals of improving student communication skills and their ability to work in a team as a cohesive unit in understanding and solving clinically related problems. The course incorporates a student-centered philosophy, via TBL and self-study, while keeping some of the traditional didactic and pen-on-paper methods of teaching and learning. It also presents material that is immediately relevant to the student learning, understanding and development as physicians in training and combines concepts from multiple sources into a concise, consolidated, well-received course that fulfills the medical school’s mission of integrating basic science concepts into clinical problem solving.
While Clinical Applications maximizes small group learning within a large group setting, it requires a high-level of faculty dedication and administrative support. Specifically, the faculty time commitment to the course is large (meeting weekly to discuss and plan cases, as well as attendance at all of the exercises) and heavy administrative support is required for implementation of the sessions and collation and correlation of cases, exams and grades. Nevertheless, the time invested has fostered increased communication between all first-year course directors and has encouraged more integration within the first-year curriculum as a whole. The impact of this course on the students’ application of basic science principles to clinical situations when they reach their required clinical clerkships remains to be measured. The students who experienced Clinical Applications during the 2007 academic year will begin their clinical clerkships in 2009. Therefore, another critical assessment of the course design will be the overall impact of this course on the medical education, training and competence of these students.
ACKNOWLEDGMENTS
We gratefully acknowledge Rebecca L. Cox, Ph.D., Nachum Dafny, Ph.D., and Judianne Kellaway, M.D., for helping to develop and facilitate some of the Clinical Applications sessions. We gratefully acknowledge Elizabeth Green and Wai-San Johansson for their invaluable help in the administration of the course. Development of the course was supported in part from a Master Teacher Award provided by the Office of Educational Programs of The University of Texas Medical School at Houston. This study was reviewed by the UTHSC-Houston Committee for the Protection of Human Subjects and determined to be exempt (HSC-MS-07-0127).
REFERENCES
- 1.Patel, V.L., Yoskowitz, N.A., and Arocha, J.F. Towards effective evaluation and reform in medical education: a cognitive and learning sciences perspective. Advances in Health Sciences Education.2008; http://www.springerlink.com/content/5884226l0448622r/fulltext.html [Access date: 9 February, 2009].
2.Brennan, P., Dohert, C.P., McMackin, D,, Sukumaran, S., Robertson, I.H., Mangaoang, M.A., O’Mara, S.M., Mullaly, S.L, Hayden, J., Prendergast, J., and Fitzsimons, M.. Radiological Society of North America. Rote Learning Improves Memory In Seniors. ScienceDaily. 2006; (http://www.sciencedaily.com/releases/2006/11/061128084444.htm). [Access date: 7 August, 2008].
3.Chessell, G. Medical education-using interactive learning. Journal of Audiovisual Media in Medicine. 1994; 17: 77-80.
4.Harden, R.M., Davis, M.H., and Crosby, J.R. The new Dundee medical curriculum: a whole that is greater than the sum of the parts. Medical Education. 1997; 31: 264-271.
5.Frank, J.R., and Danoff, D. The Can MEDS initiative: implementing an outcome-based framework of physician competencies. Medical Teacher. 2007; 29: 642-647.
6.Graham, M.J., Naqvi, Z., Encandela, J.A., Bylund, C.L., Dean, R., Calero-Breckheimer, A., and Schmidt, H.J. What indicates competency in systems based practice? An analysis of perspective consistency among healthcare team members. Advances in Health Sciences Education. 2008; (http://www.springerlink.com/content/9177v8055x5qr363/fulltext.pdf) [Access date: 28 February, 2008].
7.University of Texas Medical School at Houston. Core Competencies. 2005: (http://med.uth.tmc.edu/administration/edu_programs/ep/curriculum/index.htm). [Access date: 7 August, 2008.]8.Coulter, A. Editorial: Patients’ views of a good doctor. British Medical Journal. 2002; 325: 668-669.
9.Freeman, G., and Hjortdahl, P. General practice. What future for continuity of care in general practice? British Medical Journal. 1997; 314:1870.
10.Thompson, B.M., Schneider, V.F., Haidet, P., Levine, R.E., McMahon, K.K., Perkowski, L.C., and Richards, B.F. Team-based learning at ten medical schools: two years later. Medical Education. 2006; 41: 250-257.
11.Michaelsen, L.K., and Sweet, M. Fundamental principles and practices of team-based learning. Chapter 2 (pages 9-34). In: Michaelsen, L.K., Parmlee, D.X., McMahon, K.K., and Levine, R.E., (Eds). Team-based learning for health professions education. Sterling, VA: Stylus Publishing, LLC; 2008.
12.Michaelsen, L.K. Team-based learning in large classes. Chapter 11 (pages 153-167). In: Michaelsen, L.K., Knight, A.B., and Fink, L.D., (Eds). Team-based learning: a transformative use of small groups in college teaching. Sterling, VA: Stylus Publishing, LLC; 2004.
13.Haidet, P., and Fecile, M.L. Team-based learning: A promising strategy to foster active learning in cancer education. Journal of Cancer Education. 2006; 21: 125-128.
14.Clark, M.C., Nguyen, H.T., Bray, C., Levine, R.E. Team-based learning in an undergraduate nursing course. Journal of Nursing Education. 2008; 47: 111-117.
15.Levine, R.E., O’Boyle, M., Haidet, P., Lynn, D.J., Stone, M.M., Wolf, D.V., and Paniagua, F.A. Transforming a clinical clerkship with team learning. Teaching and Learning in Medicine. 2004; 16:270-275.
16.Michaelsen, L.K., Parmlee, D.X., McMahon, K.K., and Levine, R.E. (Eds). Team-based learning for health professions education. Sterling, VA: Stylus Publishing, LLC; 2008.
17. Thompson, B.M., Schneider, V.F., Haidet, P., Perkowski, L.C., and Richards, B.F. Factors influencing implementation of team-based learning in health sciences education Academic Medicine. 2007; 82:S53-56.
18.Seifert, W.E., Jr., Actor, J.K., Bick, R.J., Cleary, L.J., Cox, R., Dafny, N., Felleman, D., Johansson, W.-S., Green, E., Ownby, A.R., Weisbrodt, N., and Oakes, J.L. Clinical applications: problem solving and integration of basic science concepts using team-based learning. Journal of the International Association of Medical Science Educators. 2008; 18-1S:4.
19.Williams, G., and Lau, A. Reform of undergraduate medical teaching in the United Kingdom: a triumph of evangelism over common sense. British Medical Journal. 2004; 329: 92-94.
20.Sweet, M., and Michaelsen, L.K. How group dynamics research can inform the theory and practice of postsecondary small group learning. Educational Psychology Review. 2007; 19: 31-47.
21.Steinert, Y. Student perceptions of effective small group teaching. Medical Education. 2004; 38:286-293.
22.Christianson, C.E., McBride, R.B., Vari, R.C., Olson, L., and Wilson, H.D. From traditional to patient-centered learning: curriculum change as an intervention for changing institutional culture and promoting professionalism in undergraduate medical education. Academic Medicine. 2007; 82: 1079-1088.
23.Fink, L.D. The key ideas of team-based learning. Chapter 1 (pages 3-26). In: Michaelsen, L.K., Knight, A.B., and Fink, L.D., (Eds). Team-based learning: a transformative use of small groups in college teaching. Sterling, VA: Stylus Publishing, LLC; 2004.