ABSTRACT
Problem-based learning (PBL) is a popular teaching method in medical schools, but is resource intensive due to the large number of faculty required to serve as small group tutors. This study 1) compares the effectiveness and student satisfaction of PBL small groups tutored by physicians with groups tutored by 4th year medical students (MSIVs) and 2) examines the effect of tutoring on learning by MSIVs. Sixteen MSIV students were recruited to tutor MSII groups. Seven MSIVs participated in a separate study to analyze the amount of learning that occurred as a result of teaching. The MSII students were given a quiz after each module to measure the amount of information learned, and a satisfaction survey regarding their tutor. Additionally, the tutors completed a pre-test and a post-test of the material they taught. All data was input into SPSS, a statistical analysis package, and analyzed using an Independent Samples t-test. Results indicated that there was no statistically significant difference in mean quiz scores of the MSII students between groups (those tutored by physicians and those tutored by MSIVs). There was also no statistically significant difference between groups on any of the questions on the satisfaction survey. Furthermore, the MSIV student tutor pre- and post-test scores showed no statistically significant difference although the post-test scores were all higher than the pre-test scores. These findings support the use of MSIV students as PBL tutors. The results also indicated that MSIV students may benefit from teaching MSII students. Additionally, the results suggest that MSIV students may be better prepared and more knowledgeable as physicians when they have been in a position to teach medical students.
INTRODUCTION
Problem-based learning is an instructional method which has been described as “the use of patient problems as a context for students to learn problem-solving skills and to acquire knowledge about the basic and clinical sciences”.1 This method has grown in popularity in medical schools since first introduced in the 1960’s at McMaster medical school in Ontario, Canada.2
In the early 1990’s, Oklahoma State University Center for Health Sciences (OSU-CHS) initiated an MSII hybrid course called “Clinical Problem Solving” with four hours of lecture per week combined with an additional four hours of PBL small groups. This has been an effective and popular one with the MSII students, but is extremely resource intensive. The MSII class has had approximately 88 students each year. The optimal number in each small group is considered to be 5-7 students with one tutor (or, facilitator). This size appears to encourage the most active participation of all group members and allows for a sufficient variety of student ability and experiences.3
Due to the difficulty in recruitment of an optimal number of physicians to serve as tutors we began using MSIVs two years ago to serve as tutors. The MSIVs facilitate two mornings a week and are allowed to participate during any elective clinical rotations. They are cleared by their preceptors to be off those two mornings. This allows the MSIV students time to study the cases prior to the 2 hours of facilitating. We consider this a “mini” medical education rotation within their elective rotation. All preceptors that have been approached about this have allowed their students to participate.
The study was given exempt status by the Oklahoma State University Center for Health Sciences IRB because it was an educational intervention. The MS IVs were not given an actual grade for their pre- and post-tests. These grades were used for research purposes only and are not individually identified.
The primary objectives of this study were to 1) compare the effectiveness and student satisfaction of problem-based learning (PBL) small groups tutored by physicians with PBL groups tutored by 4th year medical students (MSIVs) and 2) compare the pre-test and post-test knowledge of MSIV students who served as facilitators for second-year medical student (MSII) courses.
Brief Literature Review
The use of fourth year medical students to teach first and second year medical students has been shown to be a practical and effective alternative to professional and faculty teachers. For example, MSIV students have served as peer tutors,4 patient models for history and physical examinations,5-7 basic science assistants,8-10 and problem-based learning facilitators.11 Furthermore, MSIV’s with prior patient model/standardized patient experience were rated higher on interpersonal communications skills such as rapport, support, and patient satisfaction.7,12
Academic results of MSI and MSII students revealed that students who were taught by MSIV preceptors did as well as students that were instructed by faculty preceptors. For instance, Haist, Wilson, Brigham, Fosson, and Blue13 found that the mean GPA of the students with faculty preceptors was 3.48 (SD=.40) while the GPA for those students taught by MSIV’s was 3.27 (SD=.36). End of course written examinations of the MSI and MSII students of MSIV preceptors was 81.9% (SD=7.1) and 80.3% (SD=7.6) for the students of the faculty preceptors.6 The results of a t-test analysis revealed that the examination score differences were not significant.
When surveyed about MSIV effectiveness, the MSI and MSII medical students reported that they 1) felt more comfortable with the MSIV preceptors than with a faculty member, 2) did more talking with the MSIV as the teacher, and 3) asked more questions of the MSIV than they would with faculty.7 Josephson and Whelan14 studied the effect of allowing a senior medical student to design his own course rather than teach an already developed course. Their results indicated that the MSI students rated the course as a positive experience, appropriate to the topic and level of material, and having an overall effectiveness rating of 9.7 based on a 10-point scale.
Preparing the MSIV for teaching has been low priority of medical schools in the past. However, with the ever increasing demand for physicians, medical schools have recently begun to concentrate on teaching the MSIV student to teach the MSI and MSII students. As indicated previously in this paper, not only is it cost effective to use MSIV students but it takes a burden off of the decreasing number of full-time medical faculty members.11 However, the majority of medical schools do not provide any teaching training to their students.15-18 As a result, MSIV students move into their residency programs unprepared for the teaching aspect of their education. Haber, Bardach, Vedanthan, Gillum, Haber, Gurpeet, and Dhaliwal19 designed a study to examine the effectiveness of providing a course to develop and enhance the teaching skills of MSIV students. The students attended four l-hour lectures in two afternoon sessions. The course presented teaching methods, student evaluation procedures, a panel of residents to answer the student questions regarding teaching, and hands-on exercises to practice their teaching skills. The results of the self-report questionnaires revealed that the students strongly supported the course and 97% agreed that such a course should be required as part of the medical curriculum.
Studies have also shown that the MSIV student benefits from teaching junior medical students. For example, Josephson and Whelan14 found that MSIV students reported in self-assessment surveys that the experience made them better able to teach when they become attending physicians. Studies examining MSIV students’ benefits from teaching indicated that the teaching improved their communications skills,7 better prepared them to teach in their residencies,19 allowed them the opportunity to interact with both faculty and residents,20 and to learn practical tips to enhance their teaching skills.18
Streips and Atlas21 observed that interaction of senior medical students with second year students, whose medical terminology skills were in the early stages, gave them an idea of how they would need to tailor their conversations with future patients.
Empirical evidence of the many social and communication benefits of teaching for the MSIV is growing. However, no studies could be found in the medical literature that quantified the learning of the MSIV students as a result of their teaching experience. The most recent finding of the learning benefits of teaching was published in the psychological literature in the 1970 and 1980’s. For example, several studies indicated that the tutor showed greater academic achievement than the student.22,23 Additionally, Morgan and Toy24 found that the tutors, when tested on the Wide Range Achievement Test, tested nine months ahead of the other students. Finally, Bargh and Schul25 found that participants in their study who taught material to others scored higher on later retention tests.
It is unknown if MSIV students learn more information by teaching MSI and MSII students than those MSIV students who do not teach others. Therefore, in addition to comparing the effectiveness and student satisfaction of problem-based learning (PBL) small groups tutored by physicians to PBL groups tutored by MSIV students, our study also compared the pre-test and post-test scores of MSIV students who served as facilitators to determine if the teaching activities of the MSIV facilitators increased their knowledge base.
Research Design
A total of 16 MSIV students at OSU-CHS were recruited to tutor Problem Based Learning (PBL) small groups of MSII students enrolled in the Clinical Problem Solving course during the 2005-2006 and 2006-2007 academic years. There were a total of 88 MSII students each academic year, divided into twelve small groups. The four modules taught were: 1) endocrine, central nervous system, musculoskeletal and dermatology, 2) renal, urinary/male and reproductive, 3) hematology and gastrohepatic, and 4) cardiovascular and respiratory. Each module lasted for a half semester, with four one-hour PBL sessions each week. During each module, two PBL groups were facilitated by MSIVs and the rest of the groups were facilitated by faculty members or community physicians.
Prior to the academic year, faculty tutors participated in 1 ½ hours of faculty development. The MSIVs were each given individual instruction on tutoring. Each of the MSIVs had been through this course as MSIIs and were familiar with the cases and PBL process.
In addition to facilitating the PBL small groups, seven of these MSIV students also participated in a separate study to analyze the amount of learning that occurred as a result of teaching. These MSIV tutors completed a pre-test and a post-test of the material they taught to the MSII students. The pre and post tests were identical to each other and contained 10 multiple choice questions. The questions were developed from important themes emphasized during the modules. The quizzes were identical to the quizzes given to MSII students. The pre and post tests were given to the student tutors immediately before and after the modules.
The MSII students were given a 10-question multiple choice quiz at the end of each module to measure the amount of information they learned. Two faculty facilitated groups were randomly selected from each module and the MSII students’ quiz scores from these groups were compared to the two MSIV facilitated groups.
The students also completed satisfaction surveys (1 = very dissatisfied, 5 = very satisfied) of the faculty and MSIV tutors.
Data Analysis
The quiz scores and satisfaction with the tutor scores from the MSII students were input into SPSS, a statistical analysis package. The quiz scores were analyzed using an Independent Samples t-test to determine if there was a significant difference in the scores of students who had a faculty tutor versus an MSIV tutor. Additionally, the MSII student tutor satisfaction data was analyzed using a t-test to determine if there was a difference in satisfaction for the faculty versus MSIV tutors.
The MSIV student pre/post tests also were analyzed using a t-test. Specifically, the MSIV post-test scores were compared to their pre-test quiz scores to determine if they knew more information after teaching it to others.
RESULTS
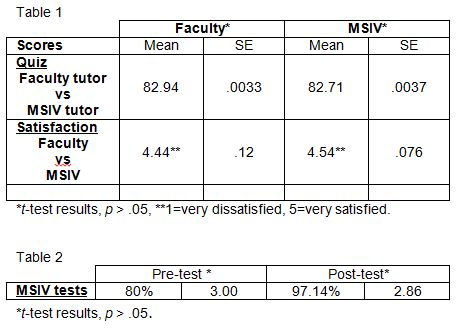
1) Quiz scores. There was no statistically significant difference in mean quiz scores between groups for the two academic years (faculty-tutor M = 82.94%, SE = .0033, MSIV M = 82.71%, SE = .0037p greater than .05).
2) Satisfaction scores. There was no statistically significant difference in the mean of the total score on the satisfaction survey (faculty M = 4.44, SE = .12, MSIV M = 4.54, SE = .076, p greater than .05). The comments made by MSIIs on the satisfaction survey regarding the MSIVs as tutors were consistently positive and included the following:
“Outstanding job. Was a doubter about having a student tutor, but have ended up not wanting to leave the group. She probably was a better resource and knew the material better than most of the physician tutors.”
“I really enjoyed having a med student as a tutor. She was able to give examples. Also, her knowledge of our lecture material from other classes was fresh. In her spare time she was able to give us pointers for boards and problems she experienced while adjusting to a clinical setting.”
“It was a very good experience to have the 4th year students as leaders. Not only were they able to explain material as needed, but they effectively prepared us for CPS exams, rotations, and freely offered advice about residency.”
“We should have more 4th years as tutors. Not only do they provide us with knowledge about the cases, they offer lots of information and advice about our clinical rotations as they pertain to our case topic.”
“Thoroughly enjoyed and truly appreciated having an MSIV start me off with Clinical Problem Solving. Integrated student and doctor perspective with helpful approaches and hints along the way. EXCELLENT!”
3) MSIV Pre and Post Tests. Finally, the MSIV student pre-test scores were compared to their post-test scores. All of the MSIV students received higher scores on their post-test (M= 97.14, SE = 2.86) than on their pre-test (M = 80.00, SE = 3.00) scores. However, there was no statistically significant difference in quiz scores between the pre and post-tests.
DISCUSSION
This study found that the second year medical students scored the same on quizzes regardless of whether the tutor was a physician or a fourth year medical student. In addition, satisfaction scores indicated that students were as satisfied with MSIV tutors as with faculty tutors. Comments from the MSII students indicated that they enjoyed the MSIV tutors, as well.
The results of this study also indicated that MSIV students may benefit from teaching MSII students. This result supports prior studies which found that greater academic knowledge was achieved by the teaching students. 22-25 These findings, in addition to previous findings of cost effectiveness and reduction of burden on faculty, support the use of MSIV students as tutors.
One of the limitations of this study is the low sample size of MSIV tutors, especially those who took the pre and post tests. Future studies should include a larger sample size. Additionally, the pre-test and post-test were identical in this study. This did not control for a learning effect of pre-exposed material. To control for this effect, future studies should prepare two different tests which cover the same material.
REFERENCES
- 1. Albanese, M.A., and Mitchell, S. Problem-based learning: A review of literature on its outcomes and implementation issues. Academic Medicine. 1993; 68 (1): 52-80.
2. Norman, G.A., and Schmidt, H.G. The Psychological Basis of Problem-Based Learning: A Review of the Evidence. Academic Medicine. 1992; 67 (9):557-65.
3. Barrows, H.S. Practice-Based Learning; Problem-Based Learning Applied to Medical Education. Springfield, IL: Southern Illinois University School of Medicine. 1994.
4. Goodfellow, P.B., and Schofield, E. Peer tutorials amongst medical students. Medical Education. 2001; 35:1001-1002.
5. Barnes, H.V., Albanese, M., Schroeder, J., and Reiter, S. Senior medical students teaching the basic skills of history and physical examination. Journal of Medical Education. 1978; 53: 432-434.
6. Haist, S.A., Wilson, J.F., Fosson, S.E., and Brigham, N.L. Are fourth-year medical students effective teachers of the physical examination of first-year medical students? Journal of General Internal Medicine. 1997; 12:177-181.
7. Blatt, B., and Greenberg, L. A multi-level assessment of a program to teach medical students to teach. Advances in Health Sciences Education. 2007; 12:7-18.
8. Carroll, M. Peer tutoring: Can medical students teach biochemistry? Biochemical Education. 1996; 34(1):13-15.
9. Trevino, F.M., and Eiland, D.C. Evaluation of a basic science, peer tutorial program for first- and second-year medical students. Journal of Medical Education. 1980; 55:952-953.
10. Walker-Bartnick, L.A., Berger, J.H., and Kapelman, M.M. A model for peer tutoring in the medical school setting. Journal of Medical Education. 1984; 52:520-522.
11. Clark, L.C, Eddy, W.S., Stone, S.M., Thomason, D.E., and Thurman, C.C. Tutorless PBL groups in a medical school. Academic Exchange Quarterly. 2006; 10(4): 205-210.
12. Sasson, V.A, Blatt, B., Kallenberg, G., Delaney, M. and White, F. “Teach 1, Do 1…Better”: Superior communication skills in senior medical students serving as standardized patient-examiners for their junior peers. Academic Medicine. 1999; 74(8):932-937.
13. Haist, S.A., Wilson, J.F., Brigham, N.L., Fosson, S.E., and Blue, A.V. Comparing fourth year medical students with faculty in the teaching of physical examination skills to first-year students. Academic Medicine. 1998; 73(2):198-200.
14. Josephson, S.A., and Whelan, A.J. A new first-year course designed and taught by a senior medical student. Academic Medicine. 2002; 77(12):1207-1211.
15. Paiva, R.E.A., Kienzler, L.M., and Anderson, M.B. Preparation for the teaching role in residencies: An elective for medical students. Journal of Medical Education. 1982; 57:792-794.
16. Greenberg, L.W., and Jewett, L.S. Preparing medical students to teach: an educational program using three approaches. Medical Teaching,. 2002; 9:409-414.
17. Pasquale, S.J., and Pugnaire, M.P. Preparing medical students to teach. Academic Medicine. 2002; 77:1175-1176.
18. Bardach, N.S., Vedanthan, R., and Haber, R. J. ‘Teaching to Teach’: enhancing fourth year medical students’ teaching skills. Really Good Stuff: Reports of new ideas in medical education. In: M.B. Anderson (Ed.). Blackwell Publishing Ltd. 2003.
19. Haber, R.J., Bardach, N.S., Vedanthan, R., Gillum, L.A., Haber, L.A., and Dhaliwal, G.S. Preparing fourth-year medical students to teach during internship. Journal of General Internal Medicine. 2006; 2:518-520.
20. Greenberg, L.W., Goldberg, R.M. and Jewett, L.S. Teaching in the clinical setting: factors influencing residents’ perceptions, confidence, and behavior. Medical Education. 1984; 18:360-365.
21. Streips, U.N., and Atlas, R. M. Fourth Year Medical Students are Effective Case Discussion Leaders. Journal of the International Association of Medical Science Educators. 2001; 10: 23-26.
22. Allen, V.L., and Feldman, R.S. Learning through tutoring: Low achieving children as tutors. Journal of Experimental Education. 1973; 42:1-5.
23. Johnson, K.R., Sulzer-Azarolff, B., and Maass, C.A. The effects of internal proctoring upon examination performance in a personalized instruction course. Journal of Personalized Instruction. 1977; 1:113-117.
24. Morgan, R.F., and Toy, T.B. Learning by teaching: A student-to-student compensatory tutoring program in a rural school system and its relevance to the educational cooperative. Psychological Record. 1970; 20:159-169.