Abstract
An innovative and educationally sound method was introduced at the University of Louisville, School of Medicine for the education of the second year medical students. Instruction is by physicians, who present a clinical case in the Socratic manner. A group of students, through questioning, derive important facts about the case and ultimately agree on a differential diagnosis for the patient described in the case. The students then spend individual time arriving at the diagnosis of the disease and submit a report on their research. This information is shared with the entire class. This novel approach is amenable for use in other medical school years, as well.
Introduction
Extensive research on student learning has been conducted and has revealed that students learn most effectively (in ways that have sustained and substantial influence on the way they think, act, and feel) when at least five conditions prevail: 1) when they are trying to solve problems or answer questions that they regard as important, intriguing, or beautiful; 2) when they are able to do so in a challenging yet supportive environment in which they can feel a strong sense of control over their own education; 3) when they can work collaboratively with other learners to grapple with the problems; 4) when they believe that their work will be considered fairly and honestly; and 5) when they can try, fail, and receive feedback from expert learners in advance of and separate from any summative judgment of their efforts. This summation is distilled from the work described in ref.1-18
Excellence in Basic Sciences (EBS) was formulated on the basis of the research described above and matches all the criteria listed for optimal learning conditions. It is a method designed for putting medical students into a situation of nonthreatening discovery, relevant and cooperative learning, and group and individual problem solving.
Methods
The cases
A clinical case illustrating a particular organ system is developed for the series. This includes a write-up of the case, attachment of appropriate history of present illness, relevant symptoms, physical findings, laboratory tests, imaging studies, and anything else that leads to a definition of the medical cause of the case. Then, after the solution is developed, all of the relevant basic science facts, which relate to the case are added (Figure 1).
The complete case is made available to the physician presenters. However, only the stem of the case describing the patient and complaint which brings the patient to the physician is distributed to the students (in this instance the second year medical class) by email.
The presenters
Physicians at various stages of their career are recruited to present the case to medical students (described in results).
The session
Students come to the session with the case. The physician opens with the question: “What do you want to know?” The physician only provides answers for questions asked by the students. As the questioning proceeds, the history, physical examination, tests ordered and available results are revealed, if requested. In the beginning sessions, the physician may prompt the students to make sure all relevant data are covered in the discussion. Later sessions reveal that the students have acquired a very efficient data seeking methodology. The physician then helps the students develop a differential diagnosis based on what has been revealed. Often this involves discussion among the students who are present at the session. The students are left with several differential possibilities, including the true solution to the case. Ideally, the students then do their own research to come up with the diagnosis and support their findings. They email the solution to the course director within three days (Figure 2). As an added benefit, a cost analysis of what the students “ordered” can be presented to the class to expose them to the reality of medical costs (Figure 3).


The solution to the case
The complete solution is posted a few days later for the class to review and copy if needed. Also, the solutions offered by students are posted along with the case for everyone to review.
Results and Discussion
During the last two academic years, 57 voluntary Excellence in Basic Sciences (EBS) sessions have been done at the University of Louisville School of Medicine. The sessions occurred each Wednesday at noon, except during examination weeks and vacation time. The attendance varied with the sessions and the other events occurring at the medical school (ranging between 10 and 40 students per session/class of 140). There was a core of students that did not miss a session. There were several who came to most of them. Other students attended some sessions but not others, as time permitted. However, as shown in Figure 4a, the worth of these sessions was high for everyone who completed the survey and who attended the sessions. The overall effectiveness was rated as very high (Figure 4b). Since only a fraction of the class participated in this voluntary activity, the results may be skewed by the fact that motivated students, who would benefit most from these sessions, participated most and rated it well. This cannot be disproved, though experience has shown that students who are not at the top of the class have also come to the sessions regularly and even if not visibly participating, still took careful notes and presumably benefited from the exercise.


A minority of the students turned in reports, though some did it regularly. Many more copy the posted case, solution and basic science correlation. Some request that the solution be emailed to them. Many keep a portfolio of these cases and use it as a study aid. The students can interact with EBS at three levels-active research and solution of the case, passive note taking and copy of the solutions, or just listen to the presentation and derive knowledge of the clinical discovery mechanism. All are valid responses to the EBS series. More students would participate, if there were not competing events at lunchtime and the pressures of block exams at our school. Other schools may choose to operate a similar series at a different time of day.
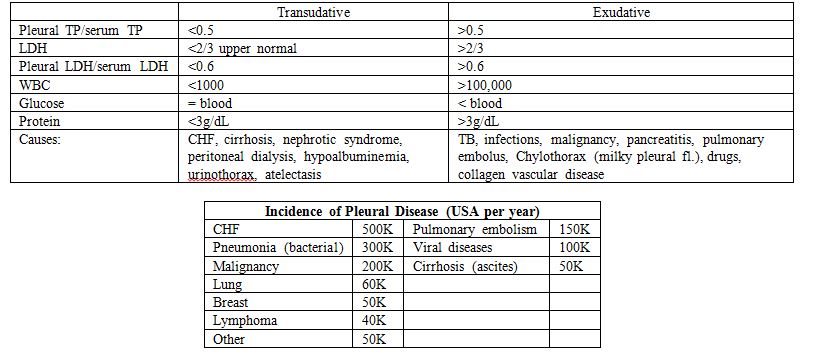
In the last academic year we ran sessions on: kidney stones, MS, portal hypertension, idiopathic myelodysplasia, inflammatory bowel disease, PHH, Von Willebrand’s Disease, acute pancreatitis, chronic granulomatous disease, myelodysplastic syndrome, pleural disease, tic doulourex, osteomalacia, juvenile rheumatoid arthritis, arsenic poisoning, Von Gierke’s disease, hypothalamic amenorrhea, Munchausen’s syndrome, depression after MI, sarcoidosis, Legionnaire’s disease, pheochromocytoma, CMV colitis and clostridium difficile in AIDS, jaundice-neonatal and estrogen induced cholestasis, protein malnutrition-kwashiorkor, pancreatic-pleural fistula compounded by chronic pancreatitis and onset diabetes, and bioterrorism.
The faculty who ran these sessions ranged from residents and chief residents in Family Medicine, Pediatrics, Internal Medicine, and Medicine to faculty in Pediatrics, Medicine, Surgery, Family Medicine and Psychiatry. We also had the Dean of Student Affairs, the Associate Dean for Curriculum, and course directors for Pathology, CPS (Clinical preparation course) and PCC (Clinical Services). The sessions worked with no formal preparation of the faculty. They all received the full case several days before their presentation and had time to prepare themselves for the questions the students offered. Preparation time varied from person to person but usually consumed no more than a couple of hours. Some also brought ancillary materials and also prepared some basic science explanation of what results from physical exams, labs, and devices would indicate for the patient under discussion. We have videotaped some of our presentations and intend to use them as training material for future physicians.
The whole session is student question driven and relies on the innate knowledge of the physicians to relate the relevant facts to the students. Several of the physicians presided over multiple cases, and every one of them found this to be a stimulating and “fun” experience. Every one of the presenters has volunteered to run a case next year and we have several new volunteers as well. The Dean for Student Affairs ran two sessions, one early and one later in the year. She was impressed how far the students had progressed in their discovery questions and correlations.
In sum, EBS represents an exciting, novel education technique that both the students and the presenters appreciate. The learning in these sessions is multifaceted, not only exposing the second year students to the discovery process that they will learn in detail in the third year, but also causing them to recall and fix in memory basic science facts from previous courses and relating them to medical situations. Similar sessions, adapted for the needs of the other medical school years, would also provide an attractive variant to standard lectures. We have arranged for some EBS sessions in the first medical school year, initiated a session for the transition summer between first and second years, and have already run some for the third year medical students. This method should be applicable to a variety of curricula, impacting not only those which are standard lecture driven but also providing a refreshing alternative to purely PBL-based education. It must be mentioned that an EBS session covers a clinical case with many basic science applications, but requires considerably less time and faculty effort than standard PBL cases.
References
- Brush T, Saye J. The use of embedded scaffolds with hypermedia-supported student-centered learning. J Educational Multimedia and Hypermedia. 2001; 10(4):333-56.
- Dillon A, Gabbard R. Hypermedia as an educational technology: A review of the quantitative research literature on learner comprehension, control, and style. Rev Educational Res. 1998; 68(3): 322-49.
- Cohen G, Steele CM. A barrier of mistrust: How negative stereotypes affect cross-race mentoring. In: Aronson J (ed) Improving academic achievement: Impact of psychological factors on education. San Diego, Academic Press. 2002. pp 303-27.
- Steele CM. A threat in the air: How stereotypes shape the intellectual identities and performance of women and African-Americans. American Psychologist. 1997;52:613-29.
- Langer EJ. The Power of Mindful Learning. Perseus Publishing, Cambridge, MA. 2000.
- Bransford J, Brown AL, Cocking RR. How People Learn: Brain, Mind, Experience, and School: Nat. Academy Press, Washington DC. 2000.
- Kamins ML, Dweck CS. Person versus process praise and criticism: Implications for contingent self-worth and coping. Dev. Psychol. 1999; 35(3):835-47.
- Butler R. Enhancing and undermining intrinsic motivation: The effects of task-involving evaluation on interest and performance. British Journal of Educational Psychology. 1988;79:474-92.
- Deci EL. Effects of externally mediated rewards on intrinsic motivation. Journal of Personality and Social Psychology. 1971;18:105-15.
- Deci EL, Ryan RM. The support of autonomy and the control of behavior. Journal of Personality and Social Psychology.1987;36:451-62.
- Schunk DH. Self-regulation of self-efficacy and attributions in academic settings. In Schunk DH, Zimmerman BJ (eds). Self-regulation of learning and performance: Issues and educational applications. Erlbaum, Hillsdale NJ. 1994. pp 75-99.
- Heyman GD, Dweck CS. Achievement goals and intrinsic motivation: Their relation and their role in adaptive motivation. Motivation and Emotion. 1992;16(3):231-47.
- Van den Hurk MM, Dolmans, D, Wolfhagen, I, Van der Vleute C. Quality of student-generated learning issues in a problem-based curriculum. Medical Teacher. 2001; 23(6):567-71.
- Peterson M. A team-based approach to problem-based learning:An evaluation of structured team problem solving. Journal of Excellence College Teaching 1996;7(3):129-53.
- Hmelo C. Problem-based learning: Effects on the early acquisition of cognitive skill in medicine. Journal of Learning Science. 1998;7(2):173-208.
- Dods R. An action research study of the effectiveness of problem-based learning in promoting the acquisition and retention of knowledge. Journal of Education of the Gifted. 1997; 20(4):423-37.
- Vernon D, Blake R. Does problem-based learning work? A meta-analysis of evaluative research. Academic Medicine. 1993; 68(7):550-63.
- Bain, K. What do the best teachers do: A fifteen year study of the thinking and practices of highly successful educators (publication pending).
- Criner, G.J, and G.E. D’Alonzo. 1999. Pulmonary Pathophysiology. Fence Creek Publishing (Madison, CN).
- Internal Medicine (fourth edition). Jay H. Stein, Editor in Chief. 1994. Mosby-Year Book, Inc. (St. Louis, MO).